
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- Cardiovascular risk/Epidemiology
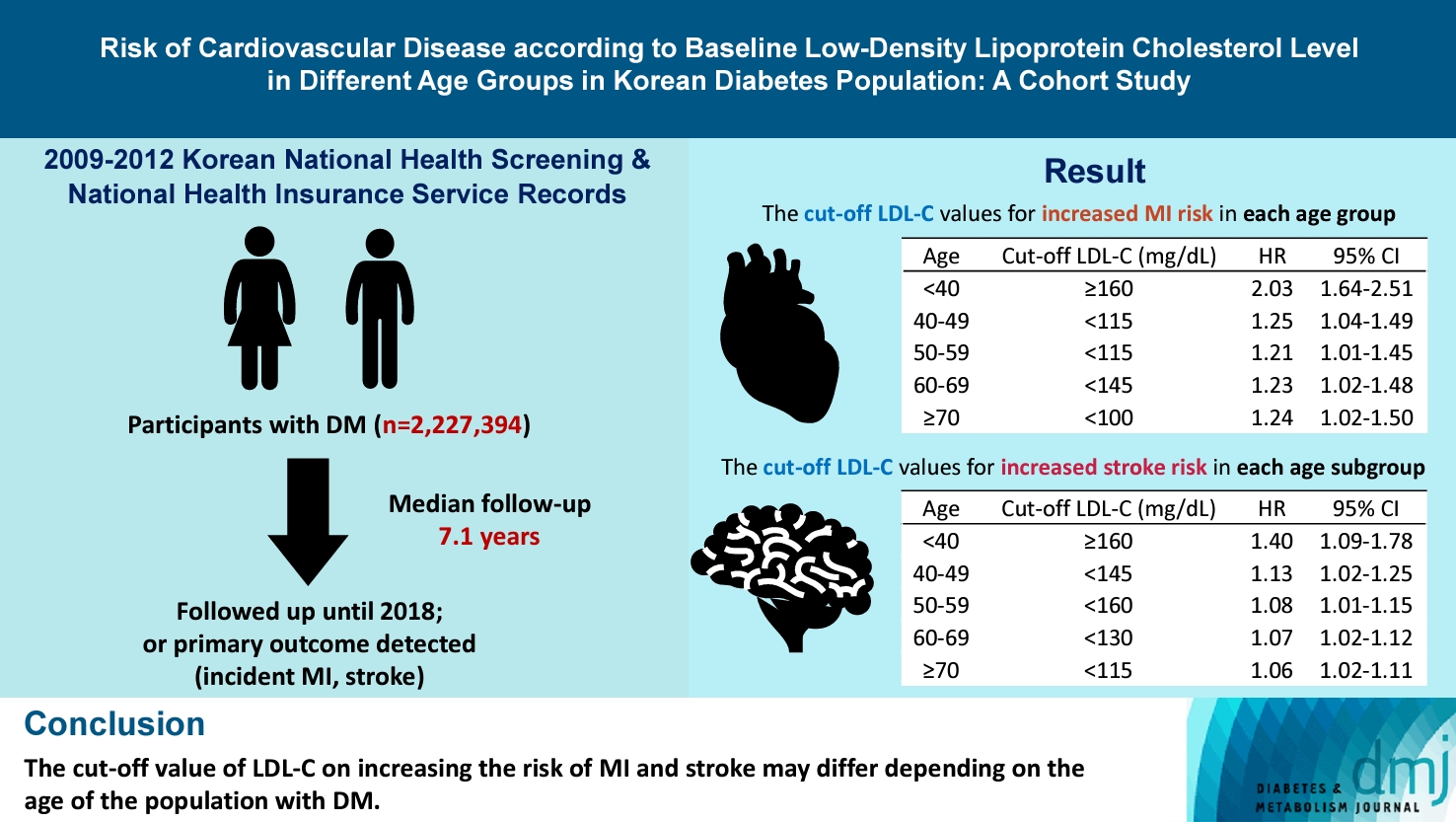
- Risk of Cardiovascular Disease according to Baseline Low-Density Lipoprotein Cholesterol Level in Different Age Groups in Korean Diabetes Population: A Cohort Study
- Tae Kyung Yoo, Kyung-Do Han, Eun-Jung Rhee, Won-Young Lee
- Diabetes Metab J. 2024;48(2):265-278. Published online February 26, 2024
- DOI: https://doi.org/10.4093/dmj.2022.0443
- 739 View
- 145 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
The association between low-density lipoprotein (LDL-C) levels and cardiovascular disease (CVD) risk in different age groups within the diabetes mellitus (DM) population remains unclear. The cohort study was conducted to investigate this relationship.
Methods
We assessed the 2009 to 2012 Korean National Health Screening and National Health Insurance Service records, with follow-up to the primary outcome (myocardial infarction [MI] or stroke) or December 2018. After excluding the participants with a history of MI or stroke, 2,227,394 participants with DM were included and categorized according to baseline LDL-C levels and age. Cox proportional hazards modeling was conducted. The CVD risk of age <40 years and LDL-C <70 mg/dL was set as the reference. In each age group, LDL-C <70 mg/dL was used as a reference for the subgroup analysis.
Results
The cut-off LDL-C value for increased MI risk in each age group varied (<40 years old, LDL-C ≥160 mg/dL: hazard ratios [HR], 2.03; 95% confidence interval [CI], 1.644 to 2.506) (40–49-year-old, LDL-C <115 mg/dL: HR, 1.245; 95% CI, 1.04 to 1.489) (50–59-year-old, LDL-C <115 mg/dL: HR, 1.21; 95% CI, 1.014 to 1.445) (60-69-year-old, LDL-C <145 mg/dL: HR, 1.229; 95% CI, 1.022 to 1.479) (≥70 years old group, LDL-C <100 mg/dL: HR, 1.238; 95% CI, 1.018 to 1.504). The cut-off LDL-C values for increased stroke risk varied in each age subgroup (<40 years old, LDL-C ≥160 mg/dL: HR, 1.395; 95% CI, 1.094 to 1.779) (40–49-year-old, LDL-C <145 mg/dL: HR, 1.13; 95% CI, 1.019 to 1.253) (50–59-year-old, LDL-C <160 mg/dL: HR, 1.079; 95% CI, 1.008 to 1.154) (60–69-year-old, LDL-C <130 mg/dL: HR, 1.07; 95% CI, 1.022 to 1.119) (≥70 years old, LDL-C <115 mg/dL: HR, 1.064; 95% CI, 1.019 to 1.112).
Conclusion
The effect of LDL-C on the risk of CVD differs depending on the age of the population with DM.
- Complications
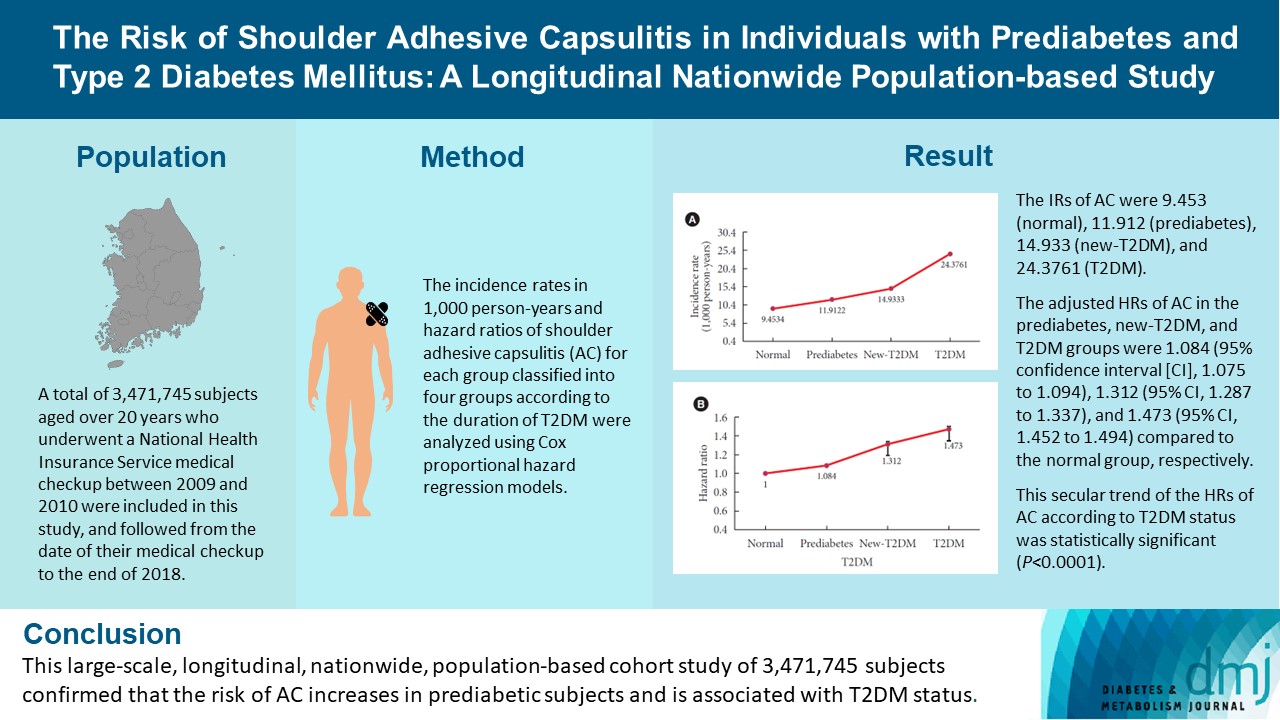
- The Risk of Shoulder Adhesive Capsulitis in Individuals with Prediabetes and Type 2 Diabetes Mellitus: A Longitudinal Nationwide Population-Based Study
- Jong-Ho Kim, Bong-Seoung Kim, Kyung-do Han, Hyuk-Sang Kwon
- Diabetes Metab J. 2023;47(6):869-878. Published online August 23, 2023
- DOI: https://doi.org/10.4093/dmj.2022.0275
- 1,538 View
- 145 Download
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
This study aimed to investigate the association between type 2 diabetes mellitus (T2DM) and shoulder adhesive capsulitis (AC) using a large-scale, nationwide, population-based cohort in the Republic of Korea.
Methods
A total of 3,471,745 subjects aged over 20 years who underwent a National Health Insurance Service medical checkup between 2009 and 2010 were included in this study, and followed from the date of their medical checkup to the end of 2018. Subjects were classified into the following four groups based on the presence of dysglycemia and history of diabetes medication: normal, prediabetes, newly diagnosed T2DM (new-T2DM), and T2DM (claim history for antidiabetic medication). The endpoint was new-onset AC during follow-up. The incidence rates (IRs) in 1,000 person-years and hazard ratios (HRs) of AC for each group were analyzed using Cox proportional hazard regression models.
Results
The IRs of AC were 9.453 (normal), 11.912 (prediabetes), 14.933 (new-T2DM), and 24.3761 (T2DM). The adjusted HRs of AC in the prediabetes, new-T2DM, and T2DM groups were 1.084 (95% confidence interval [CI], 1.075 to 1.094), 1.312 (95% CI, 1.287 to 1.337), and 1.473 (95% CI, 1.452 to 1.494) compared to the normal group, respectively. This secular trend of the HRs of AC according to T2DM status was statistically significant (P<0.0001).
Conclusion
This large-scale, longitudinal, nationwide, population-based cohort study of 3,471,745 subjects confirmed that the risk of AC increases in prediabetic subjects and is associated with T2DM status. -
Citations
Citations to this article as recorded by- Impacts of preoperative anxiety and depression on pain and range of motion after arthroscopic frozen shoulder release: a cohort study
Yahia Haroun, Ahmed Saeed Younis, Wessam Fakhery Ebied, Mohamed Amr Hemida, Ahmed H. Khater
International Orthopaedics.2024;[Epub] CrossRef - SUBDIAPHRAGMATIC PHRENIC NERVE SUPPLY: A SYSTEMATIC REVIEW
María Pérez-Montalbán, Encarna García-Domínguez, Ángel Oliva-Pascual-Vaca
Annals of Anatomy - Anatomischer Anzeiger.2024; : 152269. CrossRef
- Impacts of preoperative anxiety and depression on pain and range of motion after arthroscopic frozen shoulder release: a cohort study
- Metabolic Risk/Epidemiology
- Differential Impact of Obesity on the Risk of Diabetes Development in Two Age Groups: Analysis from the National Health Screening Program
- Tae Kyung Yoo, Kyung-Do Han, Yang-Hyun Kim, Ga Eun Nam, Sang Hyun Park, Eun-Jung Rhee, Won-Young Lee
- Diabetes Metab J. 2023;47(6):846-858. Published online August 23, 2023
- DOI: https://doi.org/10.4093/dmj.2022.0242

- 1,199 View
- 143 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
The effect of obesity on the development of type 2 diabetes mellitus (DM) in different age groups remains unclear. We assessed the impact of obesity on the development of DM for two age groups (40-year-old, middle age; 66-year-old, older adults) in the Korean population.
Methods
We analyzed Korean National Health Insurance Service data of 4,145,321 Korean adults with 40- and 66-year-old age without DM, between 2009 and 2014. Participants were followed up until 2017 or until the diagnosis of DM. We assessed the risk of DM based on the body mass index and waist circumference of the participants. Multiple confounding factors were adjusted.
Results
The median follow-up duration was 5.6 years. The association of general and abdominal obesity with the risk of DM development was stronger in the 40-year-old group (general obesity: hazard ratio [HR], 3.566, 95% confidence interval [CI], 3.512 to 3.622; abdominal obesity: HR, 3.231; 95% CI, 3.184 to 3.278) than in the 66-year-old group (general obesity: HR, 1.739; 95% CI, 1.719 to 1.759; abdominal obesity: HR, 1.799; 95% CI, 1.778 to 1.820). In the 66-year-old group, abdominal obesity had a stronger association with the development of DM as compared to general obesity. In the 40-year-old group, general obesity had a stronger association with the risk of DM development than abdominal obesity.
Conclusion
The influence of general and abdominal obesity on the development of DM differed according to age. In older adults, abdominal obesity had a stronger association with DM development than general obesity.
- Guideline/Fact Sheet
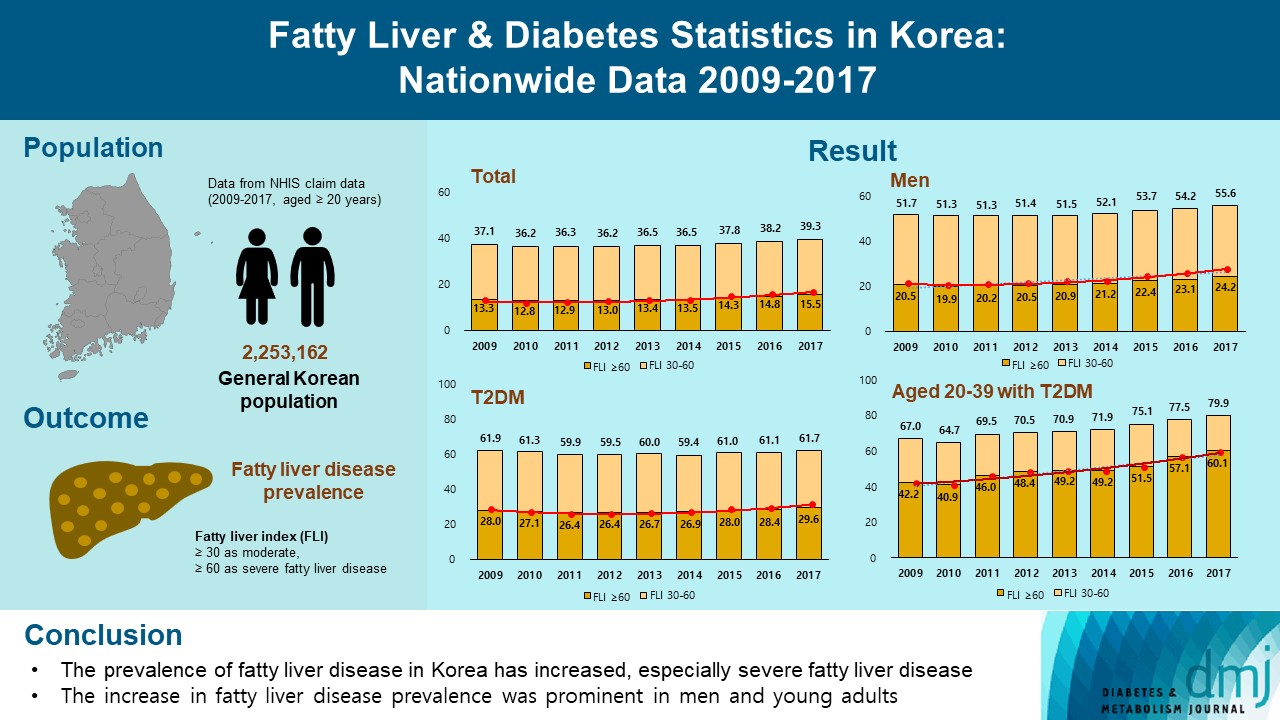
- Fatty Liver & Diabetes Statistics in Korea: Nationwide Data 2009 to 2017
- Eugene Han, Kyung-Do Han, Yong-ho Lee, Kyung-Soo Kim, Sangmo Hong, Jung Hwan Park, Cheol-Young Park, on Behalf of Fatty Liver Research Group of the Korean Diabetes Association
- Diabetes Metab J. 2023;47(3):347-355. Published online March 29, 2023
- DOI: https://doi.org/10.4093/dmj.2022.0444
- 3,559 View
- 207 Download
- 5 Web of Science
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
This study investigated the changes of fatty liver disease prevalence in general Korean population.
Methods
This study analyzed data from the Korean National Health Insurance Service from 2009 to 2017 that included individuals aged 20 years or older who had undergone a medical health examination. Fatty liver disease was assessed using the fatty liver index (FLI). The disease severity was defined by FLI cutoff, ≥30 as moderate, and ≥60 as severe fatty liver disease.
Results
The prevalence of Korean adults aged 20 years or over with fatty liver disease (FLI ≥60) increased from 13.3% in 2009 to 15.5% in 2017 (P for trend <0.001). The increase in fatty liver disease prevalence was prominent in men (from 20.5% to 24.2%) and the young age (20 to 39 years) group (from 12.8% to 16.4%) (P for interaction <0.001). The prevalence of fatty liver disease was the highest in type 2 diabetes mellitus (T2DM, 29.6%) population compared to that of prediabetes or normoglycemia (10.0% and 21.8%) in 2017. The prevalence of fatty liver disease had statistically increased in individuals with T2DM and prediabetes (P for trend <0.001). Its prevalence increased more steeply in the young-aged population with T2DM, from 42.2% in 2009 to 60.1% in 2017. When applying a lower FLI cutoff (≥30) similar results were observed.
Conclusion
The prevalence of fatty liver disease in the Korean population has increased. Individuals who are young, male, and have T2DM are vulnerable to fatty liver disease. -
Citations
Citations to this article as recorded by- Longitudinal changes in fatty liver index are associated with risk of hepatocellular carcinoma: A nationwide cohort study in Korea
Min Gu Kang, Chang Hun Lee, Chen Shen, Jong Seung Kim, Ji Hyun Park
Journal of Hepatology.2024; 80(5): e216. CrossRef - Repeated detection of non‐alcoholic fatty liver disease increases the incidence risk of type 2 diabetes in young adults
Jin Hwa Kim, Young Sang Lyu, Mee Kyoung Kim, Sang Yong Kim, Ki‐Hyun Baek, Ki‐Ho Song, Kyungdo Han, Hyuk‐Sang Kwon
Diabetes, Obesity and Metabolism.2024; 26(1): 180. CrossRef - Mortality in metabolic dysfunction-associated steatotic liver disease: A nationwide population-based cohort study
Eugene Han, Byung-Wan Lee, Eun Seok Kang, Bong-Soo Cha, Sang Hoon Ahn, Yong-ho Lee, Seung Up Kim
Metabolism.2024; 152: 155789. CrossRef - Association of non-alcoholic fatty liver disease with cardiovascular disease and all cause death in patients with type 2 diabetes mellitus: nationwide population based study
Kyung-Soo Kim, Sangmo Hong, Kyungdo Han, Cheol-Young Park
BMJ.2024; : e076388. CrossRef - Hepatic Fibrosis and Cancer: The Silent Threats of Metabolic Syndrome
Scott L. Friedman
Diabetes & Metabolism Journal.2024; 48(2): 161. CrossRef - Reply to G. Wang et al
Joo-Hyun Park, Jung Yong Hong, Kyungdo Han
Journal of Clinical Oncology.2023; 41(32): 5070. CrossRef - The Role of the Fatty Liver Index (FLI) in the Management of Non-Alcoholic Fatty Liver Disease: A Systematic Review
Teodora Biciusca, Sorina Ionelia Stan, Mara Amalia Balteanu, Ramona Cioboata, Alice Elena Ghenea, Suzana Danoiu, Ana-Maria Bumbea, Viorel Biciusca
Diagnostics.2023; 13(21): 3316. CrossRef - Lean or Non-obese Nonalcoholic Fatty Liver Disease Patients: Are They Really Lean?
Eugene Han, Yong-ho Lee
Clinical and Molecular Hepatology.2023; 29(4): 980. CrossRef - Approach to Fatty Liver Disease in Patients with Type 2 Diabetes
Ji Cheol Bae
The Journal of Korean Diabetes.2023; 24(3): 107. CrossRef
- Longitudinal changes in fatty liver index are associated with risk of hepatocellular carcinoma: A nationwide cohort study in Korea
- Guideline/Fact Sheet
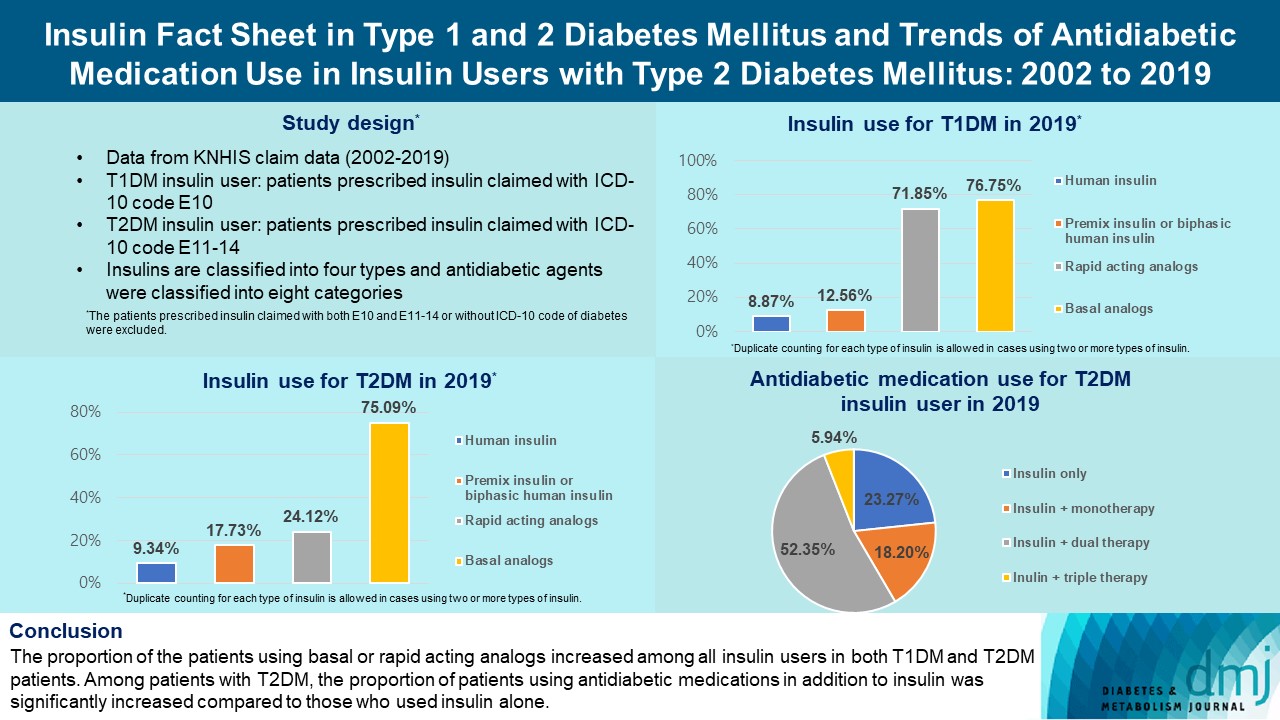
- Insulin Fact Sheet in Type 1 and 2 Diabetes Mellitus and Trends of Antidiabetic Medication Use in Insulin Users with Type 2 Diabetes Mellitus: 2002 to 2019
- Jiyun Park, Gyuri Kim, Bong-Sung Kim, Kyung-Do Han, So Yoon Kwon, So Hee Park, You-Bin Lee, Sang-Man Jin, Jae Hyeon Kim
- Diabetes Metab J. 2023;47(2):211-219. Published online February 7, 2023
- DOI: https://doi.org/10.4093/dmj.2022.0346
- 3,573 View
- 261 Download
- 1 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
This study investigated the trends of insulin use among Korean patients with type 1 diabetes mellitus (T1DM) and type 2 diabetes mellitus (T2DM). Changes in prescription of antidiabetic medications in T2DM patients taking insulin therapy were evaluated.
Methods
We analyzed data from the National Health Insurance Service database in Korea to evaluate the prevalence of insulin users and trends of insulin use in T1DM and T2DM patients from January 2002 to December 2019. We also investigated numbers and types of antidiabetic medications in insulin users with T2DM.
Results
The overall total number of insulin users increased from 2002 to 2019, reaching 348,254 for T2DM and 20,287 for T1DM in 2019 compared with 109,974 for T2DM and 34,972 for T1DM in 2002. The proportion of patients using basal analogs and short acting analogs have increased and those using human insulin, premixed insulin, or biphasic human insulin have decreased (rapid acting analogs: 71.85% and 24.12% in T1DM and T2DM, respectively, in 2019; basal analogs: 76.75% and 75.09% in T1DM and T2DM, respectively, in 2019). The use of other antidiabetic medication in addition to insulin increased for T2DM, especially in dual therapy, reaching up to 52.35% in 2019 compared with 16.72% in 2002.
Conclusion
The proportion of the patients using basal or rapid acting analogs increased among all insulin users in both T1DM and T2DM patients. Among patients with T2DM, the proportion of patients using antidiabetic medications in addition to insulin was significantly increased compared to those who used insulin alone. -
Citations
Citations to this article as recorded by- Real-World Continuous Glucose Monitoring Data from a Population with Type 1 Diabetes in South Korea: Nationwide Single-System Analysis
Ji Yoon Kim, Sang-Man Jin, Sarah B. Andrade, Boyang Chen, Jae Hyeon Kim
Diabetes Technology & Therapeutics.2024;[Epub] CrossRef - Evaluation of pharmacokinetic interactions between lobeglitazone, empagliflozin, and metformin in healthy subjects
Heeyoung Kim, Choon Ok Kim, Hyeonsoo Park, Min Soo Park, Dasohm Kim, Taegon Hong, Yesong Shin, Byung Hak Jin
Translational and Clinical Pharmacology.2023; 31(1): 59. CrossRef - Smart Insulin Pen: Managing Insulin Therapy for People with Diabetes in the Digital Era
Jee Hee Yoo, Jae Hyeon Kim
The Journal of Korean Diabetes.2023; 24(4): 190. CrossRef
- Real-World Continuous Glucose Monitoring Data from a Population with Type 1 Diabetes in South Korea: Nationwide Single-System Analysis
- Cardiovascular Risk/Epidemiology
- Cardiovascular Outcomes according to Comorbidities and Low-Density Lipoprotein Cholesterol in Korean People with Type 2 Diabetes Mellitus
- Min Kyong Moon, Junghyun Noh, Eun-Jung Rhee, Sang Hyun Park, Hyeon Chang Kim, Byung Jin Kim, Hae Jin Kim, Seonghoon Choi, Jin Oh Na, Young Youl Hyun, Bum Joon Kim, Kyung-Do Han, In-Kyung Jeong, on Behalf of the Committee of Practice Guideline of Korean Lipid and Atheroscelerosis
- Diabetes Metab J. 2023;47(1):45-58. Published online January 26, 2023
- DOI: https://doi.org/10.4093/dmj.2021.0344

- 2,973 View
- 262 Download
- 4 Web of Science
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
There are no clear data to support the cardiovascular (CV) risk categories and low-density lipoprotein cholesterol (LDL-C) treatment goals in Korean people with type 2 diabetes mellitus (T2DM). We evaluated the incidence of cardiovascular disease (CVD) according to comorbidities and suggested LDL-C treatment goals in Korean people with T2DM in nationwide cohort data.
Methods
Using the Korean National Health Insurance Service database, 248,002 people aged 30 to 90 years with T2DM who underwent routine health check-ups during 2009 were included. Subjects with previous CVD were excluded from the study. The primary outcome was incident CVD, defined as a composite of myocardial infarction and ischemic stroke during the follow-up period from 2009 to 2018.
Results
The mean age of the study participants was 59.6±10.9 years, and median follow-up period was 9.3 years. CVD incidence increased in the order of DM duration of 5 years or more (12.04/1,000 person-years), hypertension (HT) (12.27/1,000 personyears), three or more CV risk factors (14.10/1,000 person-years), and chronic kidney disease (18.28/1,000 person-years). The risk of incident CVD increased linearly from an LDL-C level of ≥70 mg/dL in most patients with T2DM. In T2DM patients without HT or with a DM duration of less than 5 years, the CVD incidence increased from LDL-C level of ≥100 mg/dL.
Conclusion
For primary prevention of CVD in Korean adults with T2DM, it can be helpful to lower LDL-C targets when there are chronic kidney disease, HT, a long duration of diabetes mellitus, or three or more CV risk factors. -
Citations
Citations to this article as recorded by- Lipid Management in Korean People with Type 2 Diabetes Mellitus: Korean Diabetes Association and Korean Society of Lipid and Atherosclerosis Consensus Statement
Ye Seul Yang, Hack-Lyoung Kim, Sang-Hyun Kim, Min Kyong Moon
Diabetes & Metabolism Journal.2023; 47(1): 1. CrossRef - Optimal Low-Density Lipoprotein Cholesterol Level for Primary Prevention in Koreans with Type 2 Diabetes Mellitus
Ji Yoon Kim, Nam Hoon Kim
Diabetes & Metabolism Journal.2023; 47(1): 42. CrossRef - Lipid Management in Korean People With Type 2 Diabetes Mellitus: Korean Diabetes Association and Korean Society of Lipid and Atherosclerosis Consensus Statement
Ye Seul Yang, Hack-Lyoung Kim, Sang-Hyun Kim, Min Kyong Moon
Journal of Lipid and Atherosclerosis.2023; 12(1): 12. CrossRef - 2023 Clinical Practice Guidelines for Diabetes: Management of Cardiovascular Risk Factors
Ye Seul Yang
The Journal of Korean Diabetes.2023; 24(3): 135. CrossRef - 2023 Clinical Practice Guidelines for Diabetes Mellitus of the Korean Diabetes Association
Jong Han Choi, Kyung Ae Lee, Joon Ho Moon, Suk Chon, Dae Jung Kim, Hyun Jin Kim, Nan Hee Kim, Ji A Seo, Mee Kyoung Kim, Jeong Hyun Lim, YoonJu Song, Ye Seul Yang, Jae Hyeon Kim, You-Bin Lee, Junghyun Noh, Kyu Yeon Hur, Jong Suk Park, Sang Youl Rhee, Hae J
Diabetes & Metabolism Journal.2023; 47(5): 575. CrossRef - Management of Dyslipidemia in Patients with Diabetes Mellitus
Kyung Ae Lee
The Journal of Korean Diabetes.2023; 24(3): 111. CrossRef - Significant Gap Between Guidelines and Practice in the Management of LDL Cholesterol: Insight From the Survey of the Korean Society of Myocardial Infarction
Sang Yeub Lee, Kyung Hoon Cho, Jang Hoon Lee, Young Joon Hong, Jin yong Hwang, Myung Ho Jeong, Weon Kim
Journal of Korean Medical Science.2023;[Epub] CrossRef
- Lipid Management in Korean People with Type 2 Diabetes Mellitus: Korean Diabetes Association and Korean Society of Lipid and Atherosclerosis Consensus Statement
- Cardiovascular Risk/Epidemiology
- Association between Low-Density Lipoprotein Cholesterol Level and Cardiovascular Outcomes in Korean Adults: A Nationwide Cohort Study
- Junghyun Noh, Min Kyong Moon, Eun-Jung Rhee, Sang Hyun Park, Hyeon Chang Kim, Byung Jin Kim, Hae Jin Kim, Seonghoon Choi, Jin Oh Na, Young Youl Hyun, Bum Joon Kim, Kyung-Do Han, In-Kyung Jeong, on Behalf of the Committee of Practice Guideline of Korean Lipid and Atheroscelerosis
- Diabetes Metab J. 2023;47(1):59-71. Published online January 26, 2023
- DOI: https://doi.org/10.4093/dmj.2021.0320

- 2,755 View
- 225 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
To validate the treatment target of low-density lipoprotein cholesterol (LDL-C) level according to the cardiovascular disease (CVD) risk which was recommended by Korean dyslipidemia guideline.
Methods
We used the Korean National Health Insurance Service database which included 3,958,048 people aged 20 to 89 years who underwent regular health screening. The primary outcome was incident CVD, defined as a composite of myocardial infarction and stroke during the follow-up period from 2009 to 2018.
Results
The risk of CVD increased from LDL-C level of 70 mg/dL in very high-risk and high-risk groups and from 130 mg/dL in moderate-risk and low-risk groups. Adjusted hazard ratios (HRs) of LDL-C ranges 70–99, 100–129, 130–159, 160–189, and ≥190 mg/dL were 1.20 (95% confidence interval [CI], 1.08–1.33), 1.27 (1.15–1.42), 1.39 (1.23–1.56), 1.69 (1.45–1.96), and 1.84 (1.49– 2.27) in very high-risk group, and 1.07 (1.02–1.13), 1.16 (1.10–1.21), 1.29 (1.22–1.36), 1.45 (1.36–1.55), and 1.73 (1.58–1.90) in high-risk group. Adjusted HRs (95% CI) of LDL-C ranges 130–159, 160–189, and ≥190 mg/dL were 1.15 (1.11–1.20), 1.28 (1.22– 1.34), and 1.45 (1.36–1.54) in moderate-risk group and 1.07 (1.02–1.13), 1.20 (1.13–1.26), and 1.47 (1.37–1.57) in low-risk group.
Conclusion
We confirmed the incidence of CVD was increased in higher LDL-C range. The risk of CVD increased from ≥70 mg/dL of LDL-C in very high-risk and high-risk groups, and from ≥130 mg/dL of LDL-C in moderate-risk and low-risk groups in Korean adults. -
Citations
Citations to this article as recorded by- Efficacy and Safety of a Single-Pill Triple Combination of Olmesartan, Amlodipine, and Rosuvastatin in Hypertensive Patients with Low-to-Moderate Cardiovascular Risk: A Multicenter, Randomized, Open-Label, Active-Control, Phase IV Clinical Trial
Byung Jin Kim, Kwang Soo Cha, Wook Hyun Cho, Eung Ju Kim, Seung-Hyuk Choi, Moo Hyun Kim, Sang-Hyun Kim, Jun-Bean Park, Seong-Mi Park, Il Suk Sohn, Kyu Hyung Ryu, In-Ho Chae
Journal of Cardiovascular Pharmacology and Therapeutics.2023;[Epub] CrossRef
- Efficacy and Safety of a Single-Pill Triple Combination of Olmesartan, Amlodipine, and Rosuvastatin in Hypertensive Patients with Low-to-Moderate Cardiovascular Risk: A Multicenter, Randomized, Open-Label, Active-Control, Phase IV Clinical Trial
- Guideline/Fact Sheet
- Diabetes Fact Sheet in Korea 2021
- Jae Hyun Bae, Kyung-Do Han, Seung-Hyun Ko, Ye Seul Yang, Jong Han Choi, Kyung Mook Choi, Hyuk-Sang Kwon, Kyu Chang Won, on Behalf of the Committee of Media-Public Relation of the Korean Diabetes Association
- Diabetes Metab J. 2022;46(3):417-426. Published online May 25, 2022
- DOI: https://doi.org/10.4093/dmj.2022.0106
- 13,840 View
- 1,659 Download
- 78 Web of Science
- 99 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
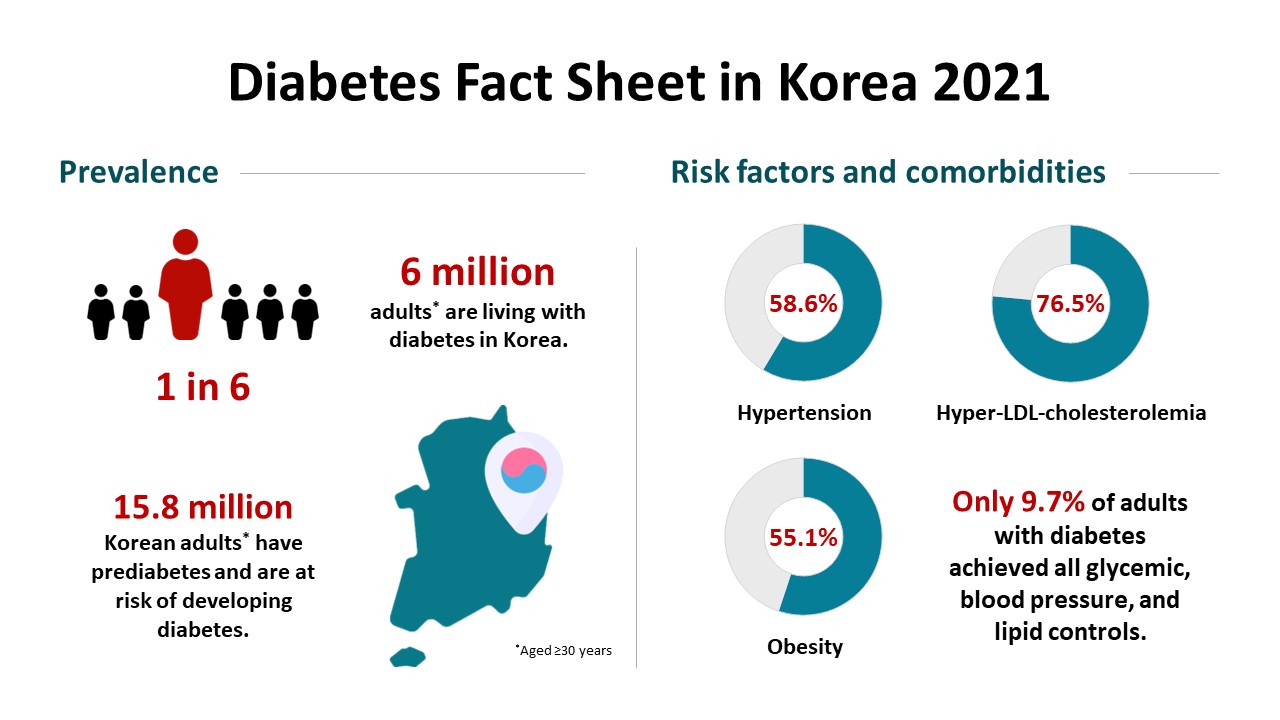
This study aimed to investigate the prevalence and management of diabetes mellitus, risk-factor control, and comorbidities among Korean adults.
Methods
We conducted a cross-sectional analysis of data from the Korea National Health and Nutrition Examination Survey to assess the prevalence, treatment, risk factors, comorbidities, and self-management behaviors of diabetes mellitus from 2019 to 2020. We also analyzed data from the Korean National Health Insurance Service to evaluate the use of antidiabetic medications in people with diabetes mellitus from 2002 through 2018.
Results
Among Korean adults aged 30 years or older, the estimated prevalence of diabetes mellitus was 16.7% in 2020. From 2019 through 2020, 65.8% of adults with diabetes mellitus were aware of the disease and treated with antidiabetic medications. The percentage of adults with diabetes mellitus who achieved glycosylated hemoglobin (HbA1c) <6.5% was 24.5% despite the increased use of new antidiabetic medications. We found that adults with diabetes mellitus who achieved all three goals of HbA1c <6.5%, blood pressure (BP) <140/85 mm Hg, and low-density lipoprotein cholesterol <100 mg/dL were 9.7%. The percentage of self-management behaviors was lower in men than women. Excess energy intake was observed in 16.7% of adults with diabetes mellitus.
Conclusion
The prevalence of diabetes mellitus among Korean adults remained high. Only 9.7% of adults with diabetes mellitus achieved all glycemic, BP, and lipid controls from 2019 to 2020. Continuous evaluation of national diabetes statistics and a national effort to increase awareness of diabetes mellitus and improve comprehensive diabetes care are needed. -
Citations
Citations to this article as recorded by- Weight change in patients with new‐onset type 2 diabetes mellitus and its association with remission: Comprehensive real‐world data
Jinyoung Kim, Bongseong Kim, Mee Kyoung Kim, Ki‐Hyun Baek, Ki‐Ho Song, Kyungdo Han, Hyuk‐Sang Kwon
Diabetes, Obesity and Metabolism.2024; 26(2): 567. CrossRef - Changes in Fatty Liver Disease and Incident Diabetes Mellitus in Young Korean Adults
Kye-Yeung Park, Hwan-Sik Hwang, Kyungdo Han, Hoon-Ki Park
American Journal of Preventive Medicine.2024; 66(4): 717. CrossRef - Widening disparities in the national prevalence of diabetes mellitus for people with disabilities in South Korea
I. Hwang, S.Y. Kim, Y.Y. Kim, J.H. Park
Public Health.2024; 226: 173. CrossRef - Questionnaire-Based Survey of Diabetes Self-Care Activities and Barriers among Young Korean Adults with Early-Onset Diabetes
Ji In Park, Sang-Wook Kim, Il Sung Nam-Goong, Kee-Ho Song, Ji Hee Yu, Ji Yun Jeong, Eun-Hee Cho
Yonsei Medical Journal.2024; 65(1): 42. CrossRef - Patients with diabetes in regions with population decline and likelihood of receiving diabetes management education and screenings for related complications in Korea
Yeong Jun Ju, Woorim Kim, Kyujin Chang, Tae Hoon Lee, Soon Young Lee
Preventive Medicine.2024; 178: 107793. CrossRef - Association between underweight and risk of heart failure in diabetes patients
Tae Kyung Yoo, Kyung‐Do Han, Eun‐Jung Rhee, Won‐Young Lee
Journal of Cachexia, Sarcopenia and Muscle.2024; 15(2): 671. CrossRef - Gastroparesis might not be uncommon in patients with diabetes mellitus in a real-world clinical setting: a cohort study
Jeongmin Lee, Hye Lim Park, Su Young Park, Chul-Hyun Lim, Min-Hee Kim, Jung Min Lee, Sang-Ah Chang, Jung-Hwan Oh
BMC Gastroenterology.2024;[Epub] CrossRef - Cumulative exposure to impaired fasting glucose and gastrointestinal cancer risk: A nationwide cohort study
Byeong Yun Ahn, Bokyung Kim, Sanghyun Park, Sang Gyun Kim, Kyungdo Han, Soo‐Jeong Cho
Cancer.2024;[Epub] CrossRef - Multidimensional behavioral factors for diabetes management among middle-aged adults: a population-based study
Hyerang Kim, Heesook Son
Journal of Public Health.2024;[Epub] CrossRef - Efficacy and Safety of Once-Weekly Semaglutide Versus Once-Daily Sitagliptin as Metformin Add-on in a Korean Population with Type 2 Diabetes
Byung-Wan Lee, Young Min Cho, Sin Gon Kim, Seung-Hyun Ko, Soo Lim, Amine Dahaoui, Jin Sook Jeong, Hyo Jin Lim, Jae Myung Yu
Diabetes Therapy.2024; 15(2): 547. CrossRef - Association between dietary selenium intake and severe abdominal aortic calcification in the United States: a cross-sectional study
Weiwei Dong, Xiaobai Liu, Lu Ma, Zhiyong Yang, Chunyan Ma
Food & Function.2024; 15(3): 1575. CrossRef - Cumulative exposure to hypertriglyceridemia and risk of type 2 diabetes in young adults
Min-Kyung Lee, Kyungdo Han, Bongsung Kim, Jong-Dai Kim, Moon Jung Kim, Byungpyo Kim, Jung Heo, Jiyeon Ahn, Seo-Young Sohn, Jae-Hyuk Lee
Diabetes Research and Clinical Practice.2024; 208: 111109. CrossRef - Recent evidence on target blood pressure in patients with hypertension
Hack-Lyoung Kim
Cardiovascular Prevention and Pharmacotherapy.2024; 6(1): 17. CrossRef - Status and trends in epidemiologic characteristics of diabetic end-stage renal disease: an analysis of the 2021 Korean Renal Data System
Kyeong Min Kim, Seon A Jeong, Tae Hyun Ban, Yu Ah Hong, Seun Deuk Hwang, Sun Ryoung Choi, Hajeong Lee, Ji Hyun Kim, Su Hyun Kim, Tae Hee Kim, Ho-Seok Koo, Chang-Yun Yoon, Kiwon Kim, Seon Ho Ahn, Yong Kyun Kim, Hye Eun Yoon
Kidney Research and Clinical Practice.2024; 43(1): 20. CrossRef -
In silico
exploration of the potential inhibitory activities of in-house and ZINC database lead compounds against alpha-glucosidase using structure-based virtual screening and molecular dynamics simulation approach
Zuhier A. Awan, Haider Ali Khan, Alam Jamal, Sulaiman Shams, Guojun Zheng, Abdul Wadood, Muhammad Shahab, Mohammad Imran Khan, Abdulaziz A. Kalantan
Journal of Biomolecular Structure and Dynamics.2024; : 1. CrossRef - Evaluation of Mobile Applications for Patients with Diabetes Mellitus: A Scoping Review
Jung Lim Lee, Youngji Kim
Healthcare.2024; 12(3): 368. CrossRef - Current status of remote collaborative care for hypertension in medically underserved areas
Seo Yeon Baik, Kyoung Min Kim, Hakyoung Park, Jiwon Shinn, Hun-Sung Kim
Cardiovascular Prevention and Pharmacotherapy.2024; 6(1): 33. CrossRef - Association of non-alcoholic fatty liver disease with cardiovascular disease and all cause death in patients with type 2 diabetes mellitus: nationwide population based study
Kyung-Soo Kim, Sangmo Hong, Kyungdo Han, Cheol-Young Park
BMJ.2024; : e076388. CrossRef - Comparison of metabolic and neurological comorbidities in Asian patients with psoriasis and atopic dermatitis
Hee Joo Yang, Mi Young Lee, Jeong Hyeon Lee, Chang Jin Jung, Woo Jin Lee, Chong Hyun Won, Mi Woo Lee, Joon Min Jung, Sung Eun Chang
Scientific Reports.2024;[Epub] CrossRef - Cancer risk according to fasting blood glucose trajectories: a population-based cohort study
Thi Minh Thu Khong, Thi Tra Bui, Hee-Yeon Kang, Jinhee Lee, Eunjung Park, Jin-Kyoung Oh
BMJ Open Diabetes Research & Care.2024; 12(1): e003696. CrossRef - Participation experience in self-care program for type 2 diabetes: A mixed-methods study
Mihwan Kim, Haejung Lee, Gaeun Park, Ah Reum Khang
Journal of Korean Gerontological Nursing.2024; 26(1): 31. CrossRef - Fasting GLP-1 Levels and Albuminuria Are Negatively Associated in Patients with Type 2 Diabetes Mellitus
Cheol-Won Jang, Tae Yang Yu, Jin Woo Jeong, Se Eun Ha, Rajan Singh, Moon Young Lee, Seungil Ro
Journal of Personalized Medicine.2024; 14(3): 280. CrossRef - The clinical relevance of a polygenic risk score for type 2 diabetes mellitus in the Korean population
Na Yeon Kim, Haekyung Lee, Sehee Kim, Ye-Jee Kim, Hyunsuk Lee, Junhyeong Lee, Soo Heon Kwak, Seunggeun Lee
Scientific Reports.2024;[Epub] CrossRef - Glycemic traits and colorectal cancer survival in a cohort of South Korean patients: A Mendelian randomization analysis
So Yon Jun, Sooyoung Cho, Min Jung Kim, Ji Won Park, Seung‐Bum Ryoo, Seung Yong Jeong, Kyu Joo Park, Aesun Shin
Cancer Medicine.2024;[Epub] CrossRef - Real-World Treatment Patterns according to Clinical Practice Guidelines in Patients with Type 2 Diabetes Mellitus and Established Cardiovascular Disease in Korea: Multicenter, Retrospective, Observational Study
Ye Seul Yang, Nam Hoon Kim, Jong Ha Baek, Seung-Hyun Ko, Jang Won Son, Seung-Hwan Lee, Sang Youl Rhee, Soo-Kyung Kim, Tae Seo Sohn, Ji Eun Jun, In-Kyung Jeong, Chong Hwa Kim, Keeho Song, Eun-Jung Rhee, Junghyun Noh, Kyu Yeon Hur
Diabetes & Metabolism Journal.2024; 48(2): 279. CrossRef - Triglyceride-glucose index predicts type 2 diabetes mellitus more effectively than oral glucose tolerance test-derived insulin sensitivity and secretion markers
Min Jin Lee, Ji Hyun Bae, Ah Reum Khang, Dongwon Yi, Mi Sook Yun, Yang Ho Kang
Diabetes Research and Clinical Practice.2024; 210: 111640. CrossRef - Real-World Outcomes of Individualized Targeted Therapy with Insulin Glargine 300 Units/mL in Insulin-Naïve Korean People with Type 2 Diabetes: TOBE Study
Eun-Gyoung Hong, Kyung-Wan Min, Jung Soo Lim, Kyu-Jeung Ahn, Chul Woo Ahn, Jae-Myung Yu, Hye Soon Kim, Hyun Jin Kim, Won Kim, Dong Han Kim, Hak Chul Jang
Advances in Therapy.2024;[Epub] CrossRef - Effect of complicated, untreated and uncontrolled diabetes and pre‐diabetes on treatment outcome among patients with pulmonary tuberculosis
Kyung Hoon Kim, Hyung Woo Kim, Yong Hyun Kim, Yeonhee Park, Sung Soo Jung, Jin Woo Kim, Jee Youn Oh, Heayon Lee, Sung Kyoung Kim, Sun‐Hyung Kim, Jiwon Lyu, Yousang Ko, Sun Jung Kwon, Yun‐Jeong Jeong, Do Jin Kim, Hyeon‐Kyoung Koo, Yangjin Jegal, Sun Young
Respirology.2024;[Epub] CrossRef - Analysis of dietary behavior and intake related to glycemic control in patients with type 2 diabetes aged 30 years or older in Korea: Utilizing the 8th Korea National Health and Nutrition Examination Survey (2019–2021)
Jin-Ah Seok, Yeon-Kyung Lee
Nutrition Research and Practice.2024; 18(2): 239. CrossRef - Management of Early-Onset Type 2 Diabetes
Jin Hwa Kim
The Journal of Korean Diabetes.2024; 25(1): 4. CrossRef - Baseline glycated albumin level and risk of type 2 diabetes mellitus in Healthy individuals: a retrospective longitudinal observation in Korea
Kang-Su Shin, Min-Seung Park, Mi Yeon Lee, Eun Hye Cho, Hee-Yeon Woo, Hyosoon Park, Min-Jung Kwon
Scandinavian Journal of Clinical and Laboratory Investigation.2024; : 1. CrossRef - The Potential Role of Presepsin in Predicting Severe Infection in Patients with Diabetic Foot Ulcers
Eun Yeong Ha, Il Rae Park, Seung Min Chung, Young Nam Roh, Chul Hyun Park, Tae-Gon Kim, Woong Kim, Jun Sung Moon
Journal of Clinical Medicine.2024; 13(8): 2311. CrossRef - Myotonic dystrophy type 1 in South Korea: a comprehensive analysis of cancer and comorbidity risks
Incheol Seo, Jin-Mo Park
Neurological Sciences.2024;[Epub] CrossRef - Risk of Pancreatic Cancer and Use of Dipeptidyl Peptidase 4 Inhibitors in Patients with Type 2 Diabetes: A Propensity Score-Matching Analysis
Mee Kyoung Kim, Kyungdo Han, Hyuk-Sang Kwon, Soon Jib Yoo
Endocrinology and Metabolism.2023; 38(4): 426. CrossRef - Diabetes screening in South Korea: a new estimate of the number needed to screen to detect diabetes
Kyoung Hwa Ha, Kyung Ae Lee, Kyung-Do Han, Min Kyong Moon, Dae Jung Kim
The Korean Journal of Internal Medicine.2023; 38(1): 93. CrossRef - Sex differences in the impact of diabetes mellitus on tuberculosis recurrence: a retrospective national cohort study
Dararat Eksombatchai, Dawoon Jeong, Jeongha Mok, Doosoo Jeon, Hee-Yeon Kang, Hee Jin Kim, Hee-Sun Kim, Hongjo Choi, Young Ae Kang
International Journal of Infectious Diseases.2023; 127: 1. CrossRef - Response to Letter to the Editor From Han and Xu: “Association Between DPP4 Inhibitor Use and the Incidence of Cirrhosis, ESRD, and Some Cancers in Patients With Diabetes”
Dae Ho Lee
The Journal of Clinical Endocrinology & Metabolism.2023; 108(4): e58. CrossRef - Lipid Management in Korean People With Type 2 Diabetes Mellitus: Korean Diabetes Association and Korean Society of Lipid and Atherosclerosis Consensus Statement
Ye Seul Yang, Hack-Lyoung Kim, Sang-Hyun Kim, Min Kyong Moon
Journal of Lipid and Atherosclerosis.2023; 12(1): 12. CrossRef - Evaluation and Management of Patients With Diabetes and Heart Failure: A Korean Diabetes Association and Korean Society of Heart Failure Consensus Statement
Kyu-Sun Lee, Junghyun Noh, Seong-Mi Park, Kyung Mook Choi, Seok-Min Kang, Kyu-Chang Won, Hyun-Jai Cho, Min Kyong Moon
International Journal of Heart Failure.2023; 5(1): 1. CrossRef - Lipid Management in Korean People with Type 2 Diabetes Mellitus: Korean Diabetes Association and Korean Society of Lipid and Atherosclerosis Consensus Statement
Ye Seul Yang, Hack-Lyoung Kim, Sang-Hyun Kim, Min Kyong Moon
Diabetes & Metabolism Journal.2023; 47(1): 1. CrossRef - Evaluation and Management of Patients with Diabetes and Heart Failure: A Korean Diabetes Association and Korean Society of Heart Failure Consensus Statement
Kyu-Sun Lee, Junghyun Noh, Seong-Mi Park, Kyung Mook Choi, Seok-Min Kang, Kyu-Chang Won, Hyun-Jai Cho, Min Kyong Moon
Diabetes & Metabolism Journal.2023; 47(1): 10. CrossRef - Risk of type 2 diabetes mellitus in catholic priests compared with general public
Youngmi Eun, Sun Myeong Ock, Se-Hong Kim, Ju Hye Chung, Se Jin Park, Churlmin Kim, Min-Kyun Im, Kyung-do Han
Acta Diabetologica.2023; 60(5): 655. CrossRef - Blood pressure control and its associated factors in patients with hypertension and type 2 diabetes
Anan S Jarab, Walid Al-Qerem, Salam Alqudah, Shrouq R Abu Heshmeh, Tareq L Mukattash, Karem H Alzoubi
Electronic Journal of General Medicine.2023; 20(3): em477. CrossRef - Prevalence and associated factors of diabetes mellitus among patients with tuberculosis in South Korea from 2011 to 2018: a nationwide cohort study
Dawoon Jeong, Jeongha Mok, Doosoo Jeon, Hee-Yeon Kang, Hee Jin Kim, Hee-Sun Kim, Jeong Mi Seo, Hongjo Choi, Young Ae Kang
BMJ Open.2023; 13(3): e069642. CrossRef - The association between nutrition label utilization and disease management education among hypertension or diabetes diagnosed in Korea using 2018 Community Health Survey: a cross-sectional study
Miran Jin, Jayeun Kim, Kyuhyun Yoon
Korean Journal of Community Nutrition.2023; 28(1): 38. CrossRef - Insulin Fact Sheet in Type 1 and 2 Diabetes Mellitus and Trends of Antidiabetic Medication Use in Insulin Users with Type 2 Diabetes Mellitus: 2002 to 2019
Jiyun Park, Gyuri Kim, Bong-Sung Kim, Kyung-Do Han, So Yoon Kwon, So Hee Park, You-Bin Lee, Sang-Man Jin, Jae Hyeon Kim
Diabetes & Metabolism Journal.2023; 47(2): 211. CrossRef - Comparison of Operational Definition of Type 2 Diabetes Mellitus Based on Data from Korean National Health Insurance Service and Korea National Health and Nutrition Examination Survey
Jong Ha Baek, Yong-Moon Park, Kyung Do Han, Min Kyong Moon, Jong Han Choi, Seung-Hyun Ko
Diabetes & Metabolism Journal.2023; 47(2): 201. CrossRef - Evaluation of pharmacokinetic interactions between lobeglitazone, empagliflozin, and metformin in healthy subjects
Heeyoung Kim, Choon Ok Kim, Hyeonsoo Park, Min Soo Park, Dasohm Kim, Taegon Hong, Yesong Shin, Byung Hak Jin
Translational and Clinical Pharmacology.2023; 31(1): 59. CrossRef - Vascular and metabolic effects of ipragliflozin versus sitagliptin (IVS) in type 2 diabetes treated with sulphonylurea and metformin: IVS study
Seon Mee Kang, Han Mi Yun, Minji Sohn, Soo Lim
Diabetes, Obesity and Metabolism.2023; 25(7): 1922. CrossRef - Diabetes and Skin Disease
Jungah Lim
The Journal of Korean Diabetes.2023; 24(1): 29. CrossRef - Revisiting the Diabetes Crisis in Korea: Call for Urgent Action
Jun Sung Moon
The Journal of Korean Diabetes.2023; 24(1): 1. CrossRef - Association between Sleep Duration and Incident Diabetes Mellitus in Healthy Subjects: A 14-Year Longitudinal Cohort Study
Jin ha Jang, Wonjin Kim, Jin Sil Moon, Eun Roh, Jun Goo Kang, Seong Jin Lee, Sung-Hee Ihm, Ji Hye Huh
Journal of Clinical Medicine.2023; 12(8): 2899. CrossRef - Exercise Frequency Reduction Is Associated With Higher Risk of Infection in Newly Diagnosed Diabetes: A Nationally Representative Cohort Study
Yohwan Lim, Hye Jun Kim, Sung Soo Yoon, Sang Jun Lee, Myeong Hoon Lee, Hyewon Park, Sun Jae Park, Seogsong Jeong, Hyun Wook Han
Journal of Korean Medical Science.2023;[Epub] CrossRef - Effects of Consuming Heat-Treated Dodamssal Brown Rice Containing Resistant Starch on Glucose Metabolism in Humans
Jiyoung Park, Sea-Kwan Oh, Miae Doo, Hyun-Jung Chung, Hyun-Jin Park, Hyejin Chun
Nutrients.2023; 15(10): 2248. CrossRef - Opening the Precision Diabetes Care through Digital Healthcare
Joonyub Lee, Jin Yu, Kun-Ho Yoon
Diabetes & Metabolism Journal.2023; 47(3): 307. CrossRef - Fatty Liver & Diabetes Statistics in Korea: Nationwide Data 2009 to 2017
Eugene Han, Kyung-Do Han, Yong-ho Lee, Kyung-Soo Kim, Sangmo Hong, Jung Hwan Park, Cheol-Young Park
Diabetes & Metabolism Journal.2023; 47(3): 347. CrossRef - Trends in the Quality of Primary Care and Acute Care in Korea From 2008 to 2020: A Cross-sectional Study
Yeong Geun Gwon, Seung Jin Han, Kyoung Hoon Kim
Journal of Preventive Medicine and Public Health.2023; 56(3): 248. CrossRef - Development and Validation of Multiple Equations for Low-Density Lipoprotein and Apolipoprotein B in Korean Patients Visiting Local Clinics and Hospitals
Rihwa Choi, Sang Gon Lee, Eun Hee Lee
Nutrients.2023; 15(12): 2786. CrossRef - The role of retinal vessel geometry as an indicator of systemic arterial stiffness assessed by cardio-ankle vascular index
Dae Joong Ma, Heesun Lee, Ji Min Choi, Hyo Eun Park, Su-Yeon Choi, Hyuk Jin Choi
Frontiers in Cardiovascular Medicine.2023;[Epub] CrossRef - Association between type 2 diabetes mellitus and depression among Korean midlife women: a cross-sectional analysis study
You Lee Yang, Eun-Ok Im, Yunmi Kim
BMC Nursing.2023;[Epub] CrossRef - Associations of updated cardiovascular health metrics, including sleep health, with incident diabetes and cardiovascular events in older adults with prediabetes: A nationwide population-based cohort study
Kyoung Hwa Ha, Dae Jung Kim, Seung Jin Han
Diabetes Research and Clinical Practice.2023; 203: 110820. CrossRef - Paradigm Shift in Management of Hyperglycemia in Patients with Type 2 Diabetes: Glucocentric versus Organ Protection
Jong Chul Won
The Journal of Korean Diabetes.2023; 24(2): 59. CrossRef - Medical nutrition therapy for diabetes mellitus
Suk Chon
Journal of the Korean Medical Association.2023; 66(7): 421. CrossRef - Prevalence and treatment status of diabetes mellitus in Korea
Hyuk-Sang Kwon
Journal of the Korean Medical Association.2023; 66(7): 404. CrossRef - The impact of diabetes status on total and site-specific cancer risk in the elderly population: A nationwide cohort study
Kyuho Kim, Bongseong Kim, Hyunho Kim, Hyung Soon Park, Yu-Bae Ahn, Seung-Hyun Ko, Kyungdo Han, Jae-Seung Yun
Diabetes Research and Clinical Practice.2023; 203: 110866. CrossRef - Response to comments of Lai et al. “Proposal of one option for patient-centered, heterogeneous selection of antidiabetic drug”
Sunyoung Kim, Sang Youl Rhee
Diabetes Research and Clinical Practice.2023; 203: 110864. CrossRef - Association of Dental Diseases and Oral Hygiene Care With the Risk of Heart Failure in Patients With Type 2 Diabetes: A Nationwide Cohort Study
Youn Huh, Jung Eun Yoo, Sang‐Hyun Park, Kyungdo Han, Seon Mee Kim, Hye Soon Park, Kyung Hwan Cho, Jin‐Soo Ahn, Sang Ho Jun, Ga Eun Nam
Journal of the American Heart Association.2023;[Epub] CrossRef - Bidirectional associations between periodontal disease and systemic diseases: a nationwide population-based study in Korea
Salma Nabila, Jaesung Choi, Ji-Eun Kim, Seokyung Hahn, In-Kyung Hwang, Tae-Il Kim, Hee-Kyung Park, Ji-Yeob Choi
Scientific Reports.2023;[Epub] CrossRef - Long-term Effectiveness of the National Diabetes Quality Assessment Program in South Korea
Ji Hye Huh, Serim Kwon, Gui Ok Kim, Bo Yeon Kim, Kyoung Hwa Ha, Dae Jung Kim
Diabetes Care.2023; 46(9): 1700. CrossRef - Refined Diagnostic Protocol for Diabetic Polyneuropathy: Paving the Way for Timely Detection
Byung-Mo Oh
Annals of Rehabilitation Medicine.2023; 47(4): 234. CrossRef - Analysis of difference in body fluid composition and dietary intake between Korean adults with and without type 2 diabetes mellitus
Yu-Gyeong Kim, Ha-Neul Choi, Jung-Eun Yim
Journal of Nutrition and Health.2023; 56(4): 377. CrossRef - 2023 Clinical Practice Guidelines for Diabetes Mellitus of the Korean Diabetes Association
Jong Han Choi, Kyung Ae Lee, Joon Ho Moon, Suk Chon, Dae Jung Kim, Hyun Jin Kim, Nan Hee Kim, Ji A Seo, Mee Kyoung Kim, Jeong Hyun Lim, YoonJu Song, Ye Seul Yang, Jae Hyeon Kim, You-Bin Lee, Junghyun Noh, Kyu Yeon Hur, Jong Suk Park, Sang Youl Rhee, Hae J
Diabetes & Metabolism Journal.2023; 47(5): 575. CrossRef - Diabetes Mellitus in the Elderly Adults in Korea: Based on Data from the Korea National Health and Nutrition Examination Survey 2019 to 2020
Seung-Hyun Ko, Kyung Do Han, Yong-Moon Park, Jae-Seung Yun, Kyuho Kim, Jae-Hyun Bae, Hyuk-Sang Kwon, Nan-Hee Kim
Diabetes & Metabolism Journal.2023; 47(5): 643. CrossRef - Management of Dyslipidemia in Patients with Diabetes Mellitus
Kyung Ae Lee
The Journal of Korean Diabetes.2023; 24(3): 111. CrossRef - Association between initial continuity of care status and diabetes-related health outcomes in older patients with type 2 diabetes mellitus: A nationwide retrospective cohort study in South Korea
Hyun Woo Jung, Woo-Ri Lee
Primary Care Diabetes.2023; 17(6): 600. CrossRef - 2023 Clinical Practice Guidelines for Diabetes
Min Kyong Moon
The Journal of Korean Diabetes.2023; 24(3): 120. CrossRef - Diagnostic performance of the fibrosis-4 index and the NAFLD fibrosis score for screening at-risk individuals in a health check-up setting
Huiyul Park, Eileen L. Yoon, Mimi Kim, Jonghyun Lee, Hye-Lin Kim, Seon Cho, Eun-Hee Nah, Dae Won Jun
Hepatology Communications.2023;[Epub] CrossRef - Risk of Cause-Specific Mortality across Glucose Spectrum in Elderly People: A Nationwide Population-Based Cohort Study
Joonyub Lee, Hun-Sung Kim, Kee-Ho Song, Soon Jib Yoo, Kyungdo Han, Seung-Hwan Lee
Endocrinology and Metabolism.2023; 38(5): 525. CrossRef - The Characteristics and Risk of Mortality in the Elderly Korean Population
Sunghwan Suh
Endocrinology and Metabolism.2023; 38(5): 522. CrossRef - Comparative Risk of Type 2 Diabetes after Gastrectomy and Endoscopic Resection for Gastric Cancer: A Nationwide Cohort Study
Yeongkeun Kwon, Jin-Won Kwon, Jiyun Kim, Dohyang Kim, Jinseub Hwang, Jane Ha, Shin-Hoo Park, Sungsoo Park
Journal of the American College of Surgeons.2023; 237(6): 902. CrossRef - Efficacy and Safety of Evogliptin Add-on Therapy to Dapagliflozin/Metformin Combinations in Patients with Poorly Controlled Type 2 Diabetes Mellitus: A 24-Week Multicenter Randomized Placebo-Controlled Parallel-Design Phase-3 Trial with a 28-Week Extensio
Jun Sung Moon, Il Rae Park, Hae Jin Kim, Choon Hee Chung, Kyu Chang Won, Kyung Ah Han, Cheol-Young Park, Jong Chul Won, Dong Jun Kim, Gwan Pyo Koh, Eun Sook Kim, Jae Myung Yu, Eun-Gyoung Hong, Chang Beom Lee, Kun-Ho Yoon
Diabetes & Metabolism Journal.2023; 47(6): 808. CrossRef - Association between diabetes mellitus and cause of death in patients with tuberculosis: A Korean nationwide cohort study
Se Hyun Kwak, Dawoon Jeong, Jeongha Mok, Doosoo Jeon, Hee-Yeon Kang, Hee Jin Kim, Hee-Sun Kim, Hongjo Choi, Young Ae Kang, Frederick Quinn
PLOS ONE.2023; 18(12): e0295556. CrossRef - Strategies to Maintain the Remission of Diabetes Following Metabolic Surgery
Mi Kyung Kim, Hye Soon Kim
Journal of Metabolic and Bariatric Surgery.2023; 12(2): 26. CrossRef - Anti-Diabetic Medications and Osteoporosis
Kyongyoung Kim
The Journal of Korean Diabetes.2023; 24(4): 173. CrossRef - The associations between changes in hepatic steatosis and heart failure and mortality: a nationwide cohort study
Jiyun Park, Gyuri Kim, Hasung Kim, Jungkuk Lee, Sang-Man Jin, Jae Hyeon Kim
Cardiovascular Diabetology.2022;[Epub] CrossRef - Severe hypoglycemia as a risk factor for cardiovascular outcomes in patients with type 2 diabetes: is it preventable?
Seung-Hyun Ko
Cardiovascular Prevention and Pharmacotherapy.2022; 4(3): 106. CrossRef - Current Trends of Big Data Research Using the Korean National Health Information Database
Mee Kyoung Kim, Kyungdo Han, Seung-Hwan Lee
Diabetes & Metabolism Journal.2022; 46(4): 552. CrossRef - Current status of obesity treatment in Korea: based on the 2020 Korean Society for the Study of Obesity guidelines for obesity management
Eun-Jung Rhee
Journal of the Korean Medical Association.2022; 65(7): 388. CrossRef - 젊은 2형 당뇨병 환자의 관리
재현 배
Public Health Weekly Report.2022; 15(35): 2474. CrossRef - Analysis of the Association between Metabolic Syndrome and Renal Function in Middle-Aged Patients with Diabetes
Yoonjin Park, Su Jung Lee
International Journal of Environmental Research and Public Health.2022; 19(18): 11832. CrossRef - The Degree of Glycemic Control for the First Three Months Determines the Next Seven Years
Nami Lee, Dae Jung Kim
Journal of Korean Medical Science.2022;[Epub] CrossRef - Blood Pressure Target in Type 2 Diabetes Mellitus
Hyun-Jin Kim, Kwang-il Kim
Diabetes & Metabolism Journal.2022; 46(5): 667. CrossRef - Association Between DPP4 Inhibitor Use and the Incidence of Cirrhosis, ESRD, and Some Cancers in Patients With Diabetes
Yewon Na, Soo Wan Kim, Ie Byung Park, Soo Jung Choi, Seungyoon Nam, Jaehun Jung, Dae Ho Lee
The Journal of Clinical Endocrinology & Metabolism.2022; 107(11): 3022. CrossRef - Education for Insulin Injection in Elderly Diabetic Patients
Gi Yeon Lee
The Journal of Korean Diabetes.2022; 23(3): 201. CrossRef - Recent Updates on Phytoconstituent Alpha-Glucosidase Inhibitors: An Approach towards the Treatment of Type Two Diabetes
Hamdy Kashtoh, Kwang-Hyun Baek
Plants.2022; 11(20): 2722. CrossRef - Epidemiological characteristics of diabetes mellitus in Korea
Soon Young Lee
Journal of the Korean Medical Association.2022; 65(10): 640. CrossRef - Screening for Prediabetes and Diabetes in Korean Nonpregnant Adults: A Position Statement of the Korean Diabetes Association, 2022
Kyung Ae Lee, Dae Jung Kim, Kyungdo Han, Suk Chon, Min Kyong Moon
Diabetes & Metabolism Journal.2022; 46(6): 819. CrossRef - Oldies but Goodies: Thiazolidinedione as an Insulin Sensitizer with Cardioprotection
Eun-Hee Cho
Diabetes & Metabolism Journal.2022; 46(6): 827. CrossRef - The Mediating Effect of Acceptance Action in the Relationship between Diabetes Distress and Self-stigma among Old Adults with Diabetes in South Korea
Hyesun Kim, Kawoun Seo
Journal of Korean Academy of Community Health Nursing.2022; 33(4): 446. CrossRef
- Weight change in patients with new‐onset type 2 diabetes mellitus and its association with remission: Comprehensive real‐world data
- Lifestyle
- Changes in Patterns of Physical Activity and Risk of Heart Failure in Newly Diagnosed Diabetes Mellitus Patients
- Inha Jung, Hyemi Kwon, Se Eun Park, Kyung-Do Han, Yong-Gyu Park, Eun-Jung Rhee, Won-Young Lee
- Diabetes Metab J. 2022;46(2):327-336. Published online November 24, 2021
- DOI: https://doi.org/10.4093/dmj.2021.0046

- 5,405 View
- 210 Download
- 4 Web of Science
- 5 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub 
- Background
Exercise is recommended for type 2 diabetes mellitus (T2DM) patients to prevent cardiovascular disease. However, the effects of physical activity (PA) for reducing the risk of heart failure (HF) has yet to be elucidated. We aimed to assess the effect of changes in patterns of PA on incident HF, especially in newly diagnosed diabetic patients.
Methods
We examined health examination data and claims records of 294,528 participants from the Korean National Health Insurance Service who underwent health examinations between 2009 and 2012 and were newly diagnosed with T2DM. Participants were classified into the four groups according to changes in PA between before and after the diagnosis of T2DM: continuously inactive, inactive to active, active to inactive, and continuously active. The development of HF was analyzed until 2017.
Results
As compared with those who were continuously inactive, those who became physically active after diagnosis showed a reduced risk for HF (adjusted hazard ratio [aHR], 0.79; 95% confidence interval [CI], 0.66 to 0.93). Those who were continuously active had the lowest risk for HF (aHR, 0.77; 95% CI, 0.62 to 0.96). As compared with those who were inactive, those who exercised regularly, either performing vigorous or moderate PA, had a lower HF risk (aHR, 0.79; 95% CI, 0.69 to 0.91).
Conclusion
Among individuals with newly diagnosed T2DM, the risk of HF was reduced in those with higher levels of PA after diagnosis was made. Our results suggest either increasing or maintaining the frequency of PA after the diagnosis of T2DM may lower the risk of HF. -
Citations
Citations to this article as recorded by- Associations Between Physical Activity and the Risk of Hip Fracture Depending on Glycemic Status: A Nationwide Cohort Study
Kyoung Min Kim, Kyoung Jin Kim, Kyungdo Han, Yumie Rhee
The Journal of Clinical Endocrinology & Metabolism.2024; 109(3): e1194. CrossRef - Evaluation and Management of Patients With Diabetes and Heart Failure: A Korean Diabetes Association and Korean Society of Heart Failure Consensus Statement
Kyu-Sun Lee, Junghyun Noh, Seong-Mi Park, Kyung Mook Choi, Seok-Min Kang, Kyu-Chang Won, Hyun-Jai Cho, Min Kyong Moon
International Journal of Heart Failure.2023; 5(1): 1. CrossRef - Evaluation and Management of Patients with Diabetes and Heart Failure: A Korean Diabetes Association and Korean Society of Heart Failure Consensus Statement
Kyu-Sun Lee, Junghyun Noh, Seong-Mi Park, Kyung Mook Choi, Seok-Min Kang, Kyu-Chang Won, Hyun-Jai Cho, Min Kyong Moon
Diabetes & Metabolism Journal.2023; 47(1): 10. CrossRef - Association of plasma brain-derived neurotrophic factor levels and frailty in community-dwelling older adults
Eun Roh, Soon Young Hwang, Eyun Song, Min Jeong Park, Hye Jin Yoo, Sei Hyun Baik, Miji Kim, Chang Won Won, Kyung Mook Choi
Scientific Reports.2022;[Epub] CrossRef - The associations between changes in hepatic steatosis and heart failure and mortality: a nationwide cohort study
Jiyun Park, Gyuri Kim, Hasung Kim, Jungkuk Lee, Sang-Man Jin, Jae Hyeon Kim
Cardiovascular Diabetology.2022;[Epub] CrossRef
- Associations Between Physical Activity and the Risk of Hip Fracture Depending on Glycemic Status: A Nationwide Cohort Study
- Metabolic Risk/Epidemiology
- Dose-Dependent Effect of Smoking on Risk of Diabetes Remains after Smoking Cessation: A Nationwide Population-Based Cohort Study in Korea
- Se Eun Park, Mi Hae Seo, Jung-Hwan Cho, Hyemi Kwon, Yang-Hyun Kim, Kyung-Do Han, Jin-Hyung Jung, Yong-Gyu Park, Eun-Jung Rhee, Won-Young Lee
- Diabetes Metab J. 2021;45(4):539-546. Published online March 4, 2021
- DOI: https://doi.org/10.4093/dmj.2020.0061

- 7,718 View
- 188 Download
- 9 Web of Science
- 12 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub 
- Background
This study aimed to evaluate the dose-dependent effects of smoking on risk of diabetes among those quitting smoking.
Methods
We analyzed clinical data from a total of 5,198,792 individuals age 20 years or older who received health care check-up arranged by the national insurance program of Korea between 2009 and 2016 using the Korean National Health Insurance Service database. Cumulative smoking was estimated by pack-years. Smokers were classified into four categories according to the amount of smoking: light smokers (0.025 to 5 smoking pack-years), medium smokers (5 to 14 smoking pack-years), heavy smokers (14 to 26 smoking pack-years), and extreme smokers (more than 26 smoking pack-years).
Results
During the study period, 164,335 individuals (3.2% of the total population) developed diabetes. Compared to sustained smokers, the risk of diabetes was significantly reduced in both quitters (hazard ratio [HR], 0.858; 95% confidence interval [CI], 0.838 to 0.878) and nonsmokers (HR, 0.616; 95% CI, 0.606 to 0.625) after adjustment for multiple risk factors. The risk of diabetes gradually increased with amount of smoking in both quitters and current smokers. The risk of diabetes in heavy (HR, 1.119; 95% CI, 1.057 to 1.185) and extreme smokers (HR, 1.348; 95% CI, 1.275 to 1.425) among quitters was much higher compared to light smokers among current smokers.
Conclusion
Smoking cessation was effective in reducing the risk of diabetes regardless of weight change. However, there was a potential dose-dependent association between smoking amount and the development of diabetes. Diabetes risk still remained in heavy and extreme smokers even after smoking cessation. -
Citations
Citations to this article as recorded by- Dietary and other lifestyle factors and their influence on non-communicable diseases in the Western Pacific region
Xiaomin Sun, Dong Keon Yon, Tuan Thanh Nguyen, Kumpei Tanisawa, Kumhee Son, Ling Zhang, Jing Shu, Wen Peng, Yuexin Yang, Francesco Branca, Mark L. Wahlqvist, Hyunjung Lim, Youfa Wang
The Lancet Regional Health - Western Pacific.2024; 43: 100842. CrossRef - The Concentrations of Interleukin-6, Insulin, and Glucagon in the Context of Obesity and Type 2 Diabetes and Single Nucleotide Polymorphisms in IL6 and INS Genes
Magdalena Król-Kulikowska, Iwona Urbanowicz, Marta Kepinska, Mayank Choubey
Journal of Obesity.2024; 2024: 1. CrossRef - Chronic cigarette smoking is associated with increased arterial stiffness in men and women: evidence from a large population-based cohort
Omar Hahad, Volker H. Schmitt, Natalie Arnold, Karsten Keller, Jürgen H. Prochaska, Philipp S. Wild, Andreas Schulz, Karl J. Lackner, Norbert Pfeiffer, Irene Schmidtmann, Matthias Michal, Jörn M. Schattenberg, Oliver Tüscher, Andreas Daiber, Thomas Münzel
Clinical Research in Cardiology.2023; 112(2): 270. CrossRef - Association between Meal Frequency and Type 2 Diabetes Mellitus in Rural Adults: A Large-Scale Cross-Sectional Study
Bota Baheti, Xiaotian Liu, Mu Wang, Caiyun Zhang, Xiaokang Dong, Ning Kang, Linlin Li, Xing Li, Songcheng Yu, Jian Hou, Zhenxing Mao, Chongjian Wang
Nutrients.2023; 15(6): 1348. CrossRef - Impaired Lung Function and Lung Cancer Incidence: A Nationwide Population-Based Cohort Study
Hye Seon Kang, Yong-Moon Park, Seung-Hyun Ko, Seung Hoon Kim, Shin Young Kim, Chi Hong Kim, Kyungdo Han, Sung Kyoung Kim
Journal of Clinical Medicine.2022; 11(4): 1077. CrossRef - Smoking cessation and risk of type 2 diabetes
Jana Malinovská, Jana Urbanová, Veronika Vejtasová, Alexandra Romanová, Sabina Pálová, Syed Taha Naeem, Jan Brož
Vnitřní lékařství.2022; 68(1): E04. CrossRef - Association between lung function and the risk of atrial fibrillation in a nationwide population cohort study
Su Nam Lee, Seung-Hyun Ko, Sung-Ho Her, Kyungdo Han, Donggyu Moon, Sung Kyoung Kim, Ki-Dong Yoo, Yu-Bae Ahn
Scientific Reports.2022;[Epub] CrossRef - Sex differences in factors associated with prediabetes in Korean adults
Jin Suk Ra
Osong Public Health and Research Perspectives.2022; 13(2): 142. CrossRef - Smoking and diabetes interplay: A comprehensive review and joint statement
Vincent Durlach, Bruno Vergès, Abdallah Al-Salameh, Thibault Bahougne, Farid Benzerouk, Ivan Berlin, Carole Clair, Jacques Mansourati, Alexia Rouland, Daniel Thomas, Philippe Thuillier, Blandine Tramunt, Anne-Laurence Le Faou
Diabetes & Metabolism.2022; 48(6): 101370. CrossRef - Impact of healthy lifestyle on the risk of type 2 diabetes mellitus in southwest China: A prospective cohort study
Yanli Wu, Xi He, Jie Zhou, Yiying Wang, Lisha Yu, Xuejiao Li, Tao Liu, Jianhua Luo
Journal of Diabetes Investigation.2022; 13(12): 2091. CrossRef - Current status of health promotion in Korea
Soo Young Kim
Journal of the Korean Medical Association.2022; 65(12): 776. CrossRef - Smoking Cessation after Diagnosis of New-Onset Atrial Fibrillation and the Risk of Stroke and Death
So-Ryoung Lee, Eue-Keun Choi, Jin-Hyung Jung, Kyung-Do Han, Seil Oh, Gregory Y. H. Lip
Journal of Clinical Medicine.2021; 10(11): 2238. CrossRef
- Dietary and other lifestyle factors and their influence on non-communicable diseases in the Western Pacific region
- Cardiovascular risk/Epidemiology
- Increased Risk of Cardiovascular Disease and Mortality in Patients with Diabetes and Coexisting Depression: A Nationwide Population-Based Cohort Study
- Inha Jung, Hyemi Kwon, Se Eun Park, Kyung-Do Han, Yong-Gyu Park, Yang-Hyun Kim, Eun-Jung Rhee, Won-Young Lee
- Diabetes Metab J. 2021;45(3):379-389. Published online December 11, 2020
- DOI: https://doi.org/10.4093/dmj.2020.0008
- 7,513 View
- 236 Download
- 22 Web of Science
- 21 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub 
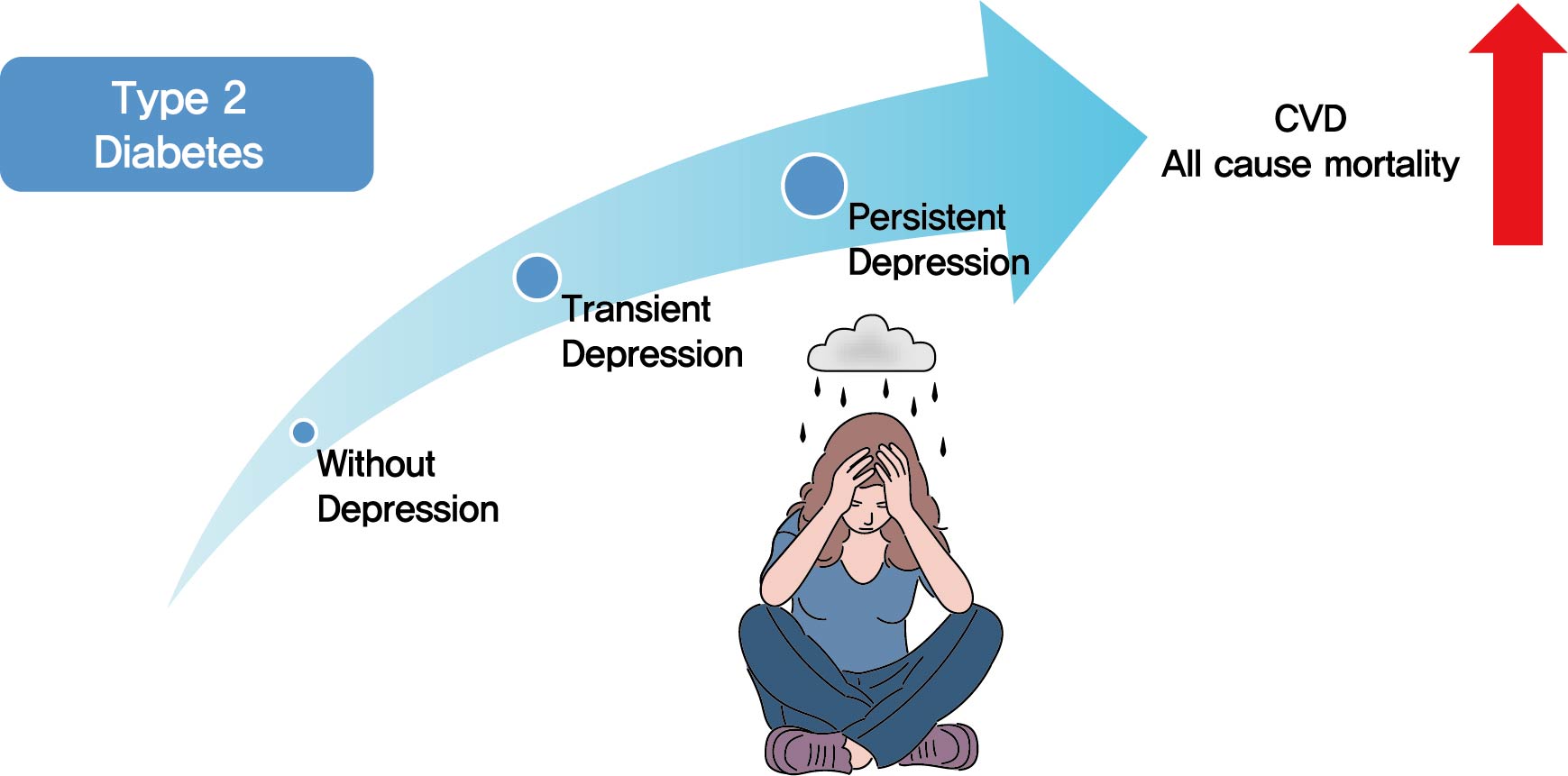
- Background
Previous studies have suggested that depression in patients with diabetes is associated with worse health outcomes. The aim of this study was to evaluate the risk of cardiovascular disease (CVD) and mortality in patients with diabetes with comorbid depression.
Methods
We examined the general health check-up data and claim database of the Korean National Health Insurance Service (NHIS) of 2,668,615 participants with type 2 diabetes mellitus who had examinations between 2009 and 2012. As NHIS database has been established since 2002, those who had been diagnosed with depression or CVD since 2002 were excluded. The 2,228,443 participants were classified into three groups according to the claim history of depression; normal group (n=2,166,979), transient depression group (one episode of depression, n=42,124) and persistent depression group (at least two episodes of depression, n=19,340). The development of CVD and mortality were analyzed from 2009 to 2017.
Results
Those with depression showed a significantly increased risk for stroke (transient depression group: hazard ratio [HR], 1.20; 95% confidence interval [CI], 1.15 to 1.26) (persistent depression group: HR, 1.54; 95% CI, 1.46 to 1.63). Those with depression had an increased risk for myocardial infarction (transient depression group: HR, 1.25; 95% CI, 1.18 to 1.31) (persistent depression group: HR, 1.38; 95% CI, 1.29 to 1.49). The persistent depression group had an increased risk for all-cause mortality (HR, 1.66; 95% CI, 1.60 to 1.72).
Conclusion
Coexisting depression in patients with diabetes has a deleterious effect on the development of CVD and mortality. We suggest that more attention should be given to patients with diabetes who present with depressive symptoms. -
Citations
Citations to this article as recorded by- Psychological resilience mediates the relationship between diabetes distress and depression among persons with diabetes in a multi-group analysis
Ajele Kenni Wojujutari, Erhabor Sunday Idemudia, Lawrence Ejike Ugwu
Scientific Reports.2024;[Epub] CrossRef - The mediating effect of depression on new-onset stroke in diabetic population: Evidence from the China health and retirement longitudinal study
Gege Jiang, Yaoling Wang, Liping Wang, Minfang Chen, Wei Li
Journal of Affective Disorders.2023; 321: 208. CrossRef - Frailty and outcomes in lacunar stroke
Sima Vazquez, Zehavya Stadlan, Justin M Lapow, Eric Feldstein, Smit Shah, Ankita Das, Alexandria F Naftchi, Eris Spirollari, Akash Thaker, Syed Faraz Kazim, Jose F Dominguez, Neisha Patel, Christeena Kurian, Ji Chong, Stephan A Mayer, Gurmeen Kaur, Chirag
Journal of Stroke and Cerebrovascular Diseases.2023; 32(2): 106942. CrossRef - Comparison of Operational Definition of Type 2 Diabetes Mellitus Based on Data from Korean National Health Insurance Service and Korea National Health and Nutrition Examination Survey
Jong Ha Baek, Yong-Moon Park, Kyung Do Han, Min Kyong Moon, Jong Han Choi, Seung-Hyun Ko
Diabetes & Metabolism Journal.2023; 47(2): 201. CrossRef - The Association between Dietary Carotenoid Intake and Risk of Depression among Patients with Cardiometabolic Disease
Jie Liang, Yuhao Wang, Min Chen
International Heart Journal.2023; 64(2): 223. CrossRef - Associations of concomitant retinopathy and depression with mortality in a nationally representative population
Zheng Lyu, Yilin Chen, Zhuoting Zhu, Xiaoyang Luo, Ying Cui, Jie Xie, Zhifan Chen, Junbin Liu, Xiyu Wu, Gabrella Bulloch, Qianli Meng
Journal of Affective Disorders.2023; 336: 15. CrossRef - Clinical insights into the cross-link between mood disorders and type 2 diabetes: A review of longitudinal studies and Mendelian randomisation analyses
Chiara Possidente, Giuseppe Fanelli, Alessandro Serretti, Chiara Fabbri
Neuroscience & Biobehavioral Reviews.2023; 152: 105298. CrossRef - Prevalence of depression and association with all-cause and cardiovascular mortality among individuals with type 2 diabetes: a cohort study based on NHANES 2005–2018 data
Zhen Feng, Wai Kei Tong, Xinyue Zhang, Zhijia Tang
BMC Psychiatry.2023;[Epub] CrossRef - Cholecystectomy Increases the Risk of Type 2 Diabetes in the Korean Population
Ji Hye Huh, Kyong Joo Lee, Yun Kyung Cho, Shinje Moon, Yoon Jung Kim, Eun Roh, Kyung-do Han, Dong Hee Koh, Jun Goo Kang, Seong Jin Lee, Sung-Hee Ihm
Annals of Surgery.2023; 278(2): e264. CrossRef - Risk of depression in patients with acromegaly in Korea (2006-2016): a nationwide population-based study
Shinje Moon, Sangmo Hong, Kyungdo Han, Cheol-Young Park
European Journal of Endocrinology.2023; 189(3): 363. CrossRef - The association between cardiovascular drugs and depression/anxiety in patients with cardiovascular disease: A meta-analysis
Lijun Zhang, Yanping Bao, Shuhui Tao, Yimiao Zhao, Meiyan Liu
Pharmacological Research.2022; 175: 106024. CrossRef - Association of mental health with the risk of coronary artery disease in patients with diabetes: A mendelian randomization study
Teng Hu, Fangkun Yang, Kewan He, Jiajun Ying, Hanbin Cui
Nutrition, Metabolism and Cardiovascular Diseases.2022; 32(3): 703. CrossRef - Comorbidity of Type 2 Diabetes Mellitus and Depression: Clinical Evidence and Rationale for the Exacerbation of Cardiovascular Disease
Mengmeng Zhu, Yiwen Li, Binyu Luo, Jing Cui, Yanfei Liu, Yue Liu
Frontiers in Cardiovascular Medicine.2022;[Epub] CrossRef - Understanding and Utilizing Claim Data from the Korean National Health Insurance Service (NHIS) and Health Insurance Review & Assessment (HIRA) Database for Research
Dae-Sung Kyoung, Hun-Sung Kim
Journal of Lipid and Atherosclerosis.2022; 11(2): 103. CrossRef - Evaluating Triglyceride and Glucose Index as a Simple and Easy-to-Calculate Marker for All-Cause and Cardiovascular Mortality
Kyung-Soo Kim, Sangmo Hong, You-Cheol Hwang, Hong-Yup Ahn, Cheol-Young Park
Journal of General Internal Medicine.2022; 37(16): 4153. CrossRef - Evaluation of rosmarinic acid against myocardial infarction in maternally separated rats
Himanshu Verma, Anindita Bhattacharjee, Naveen Shivavedi, Prasanta Kumar Nayak
Naunyn-Schmiedeberg's Archives of Pharmacology.2022; 395(10): 1189. CrossRef - Lipid cutoffs for increased cardiovascular disease risk in non-diabetic young people
Mee Kyoung Kim, Kyungdo Han, Hun-Sung Kim, Kun-Ho Yoon, Seung-Hwan Lee
European Journal of Preventive Cardiology.2022; 29(14): 1866. CrossRef - Risk factors associated with mortality among individuals with type 2 diabetes and depression across two cohorts
Christopher Rohde, Jens Steen Nielsen, Jakob Schöllhammer Knudsen, Reimar Wernich Thomsen, Søren Dinesen Østergaard
European Journal of Endocrinology.2022; 187(4): 567. CrossRef - Increased Risk of Cardiovascular Disease and Mortality in Patients with Diabetes and Coexisting Depression: A Nationwide Population-Based Cohort Study (Diabetes Metab J 2021;45:379-89)
Jin Hwa Kim
Diabetes & Metabolism Journal.2021; 45(5): 789. CrossRef - Increased Risk of Cardiovascular Disease and Mortality in Patients with Diabetes and Coexisting Depression: A Nationwide Population-Based Cohort Study (Diabetes Metab J 2021;45:379-89)
Inha Jung, Eun-Jung Rhee, Won-Young Lee
Diabetes & Metabolism Journal.2021; 45(5): 793. CrossRef - Affective Temperament and Glycemic Control – The Psychological Aspect of Obesity and Diabetes Mellitus
Natalia Lesiewska, Anna Kamińska, Roman Junik, Magdalena Michalewicz, Bartłomiej Myszkowski, Alina Borkowska, Maciej Bieliński
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2021; Volume 14: 4981. CrossRef
- Psychological resilience mediates the relationship between diabetes distress and depression among persons with diabetes in a multi-group analysis
- COVID-19
-
- Independent Impact of Diabetes on the Severity of Coronavirus Disease 2019 in 5,307 Patients in South Korea: A Nationwide Cohort Study
- Sun Joon Moon, Eun-Jung Rhee, Jin-Hyung Jung, Kyung-Do Han, Sung-Rae Kim, Won-Young Lee, Kun-Ho Yoon
- Diabetes Metab J. 2020;44(5):737-746. Published online October 21, 2020
- DOI: https://doi.org/10.4093/dmj.2020.0141
- 10,618 View
- 201 Download
- 24 Web of Science
- 23 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
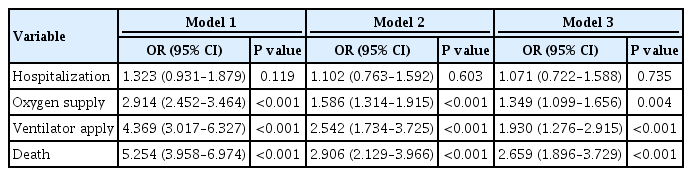
Inconsistent results have been observed regarding the independent effect of diabetes on the severity of coronavirus disease 2019 (COVID-19). We conducted a nationwide population-based cohort study to evaluate the relationship between diabetes and COVID-19 severity in South Korea.
Methods
Patients with laboratory-confirmed COVID-19 aged ≥30 years were enrolled and medical claims data were obtained from the Korean Health Insurance Review and Assessment Service. Hospitalization, oxygen treatment, ventilator application, and mortality were assessed as severity outcomes. Multivariate logistic regression analyses were performed after adjusting for age, sex, and comorbidities.
Results
Of 5,307 COVID-19 patients, the mean age was 56.0±14.4 years, 2,043 (38.5%) were male, and 770 (14.5%) had diabetes. The number of patients who were hospitalized, who received oxygen, who required ventilator support, and who died was 4,986 (94.0%), 884 (16.7%), 121 (2.3%), and 211 (4.0%), respectively. The proportion of patients with diabetes in the abovementioned outcome groups was 14.7%, 28.1%, 41.3%, 44.6%, showing an increasing trend according to outcome severity. In multivariate analyses, diabetes was associated with worse outcomes, with an adjusted odds ratio (aOR) of 1.349 (95% confidence interval [CI], 1.099 to 1.656; P=0.004) for oxygen treatment, an aOR of 1.930 (95% CI, 1.276 to 2.915; P<0.001) for ventilator use, and an aOR of 2.659 (95% CI, 1.896 to 3.729; P<0.001) for mortality.
Conclusion
Diabetes was associated with worse clinical outcomes in Korean patients with COVID-19, independent of other comorbidities. Therefore, patients with diabetes and COVID-19 should be treated with caution. -
Citations
Citations to this article as recorded by- Impact of COVID-19 on the Microbiome and Inflammatory Status of Type 2 Diabetes Patients
Gratiela Gradisteanu Pircalabioru, Georgiana Alexandra Grigore, Ilda Czobor Barbu, Mariana-Carmen Chifiriuc, Octavian Savu
Biomedicines.2023; 11(1): 179. CrossRef - Bidirectional Relationship between Glycemic Control and COVID-19 and Perspectives of Islet Organoid Models of SARS-CoV-2 Infection
Tongran Zhang, Nannan Wang, Lingqiang Zhu, Lihua Chen, Huisheng Liu
Biomedicines.2023; 11(3): 856. CrossRef - Reasons for Hospitalization Among Australians With Type 1 or Type 2 Diabetes and COVID-19
Dunya Tomic, Jonathan E. Shaw, Dianna J. Magliano
Canadian Journal of Diabetes.2023;[Epub] CrossRef - Anti-SARS-CoV-2 antibody levels predict outcome in COVID-19 patients with type 2 diabetes: a prospective cohort study
Sylvia Mink, Christoph H. Saely, Andreas Leiherer, Matthias Frick, Thomas Plattner, Heinz Drexel, Peter Fraunberger
Scientific Reports.2023;[Epub] CrossRef - Mortality-related risk factors of inpatients with diabetes and COVID-19: A multicenter retrospective study in Belgium
Thomas Servais, France Laurent, Thomas Roland, Camelia Rossi, Elodie De Groote, Valérie Godart, Ernestina Repetto, Michel Ponchon, Pascale Chasseur, Laurent Crenier, Sandrine Van Eeckhoudt, John Yango, Philippe Oriot, Mirela Morisca Gavriliu, Stéphanie Ro
Annales d'Endocrinologie.2023;[Epub] CrossRef - Screening, diagnosis and management of diabetic sensorimotor polyneuropathy in clinical practice: International expert consensus recommendations
Dan Ziegler, Solomon Tesfaye, Vincenza Spallone, Irina Gurieva, Juma Al Kaabi, Boris Mankovsky, Emil Martinka, Gabriela Radulian, Khue Thy Nguyen, Alin O Stirban, Tsvetalina Tankova, Tamás Varkonyi, Roy Freeman, Péter Kempler, Andrew JM Boulton
Diabetes Research and Clinical Practice.2022; 186: 109063. CrossRef - The Role of Diabetes and Hyperglycemia on COVID-19 Infection Course—A Narrative Review
Evangelia Tzeravini, Eleftherios Stratigakos, Chris Siafarikas, Anastasios Tentolouris, Nikolaos Tentolouris
Frontiers in Clinical Diabetes and Healthcare.2022;[Epub] CrossRef - The interrelationship between diabetes mellitus and COVID-19
ThekraAbdulaali Abed, ZainabAdil Ghani Chabuck
Medical Journal of Babylon.2022; 19(1): 1. CrossRef - Impact of Type 2 Diabetes Mellitus on the Incidence and Outcomes of COVID-19 Needing Hospital Admission According to Sex: Retrospective Cohort Study Using Hospital Discharge Data in Spain, Year 2020
Jose M. de Miguel-Yanes, Rodrigo Jimenez-Garcia, Javier de Miguel-Diez, Valentin Hernández-Barrera, David Carabantes-Alarcon, Jose J. Zamorano-Leon, Ricardo Omaña-Palanco, Ana Lopez-de-Andres
Journal of Clinical Medicine.2022; 11(9): 2654. CrossRef - Diabetes Fact Sheet in Korea 2021
Jae Hyun Bae, Kyung-Do Han, Seung-Hyun Ko, Ye Seul Yang, Jong Han Choi, Kyung Mook Choi, Hyuk-Sang Kwon, Kyu Chang Won
Diabetes & Metabolism Journal.2022; 46(3): 417. CrossRef - The burden and risks of emerging complications of diabetes mellitus
Dunya Tomic, Jonathan E. Shaw, Dianna J. Magliano
Nature Reviews Endocrinology.2022; 18(9): 525. CrossRef - Clinical Characteristics and Outcomes of Patients Hospitalized with COVID-19 at Case Hospital, Uganda
Mirriam Apiyo, Ronald Olum, Amina Kabuye, Betty Khainza, Anne M. Amate, Vittal Byabashaija, Derrick Nomujuni, Kato Sebbaale, Peter Senfuka, Simon Kazibwe, Gurav Sharma, Lindsay Davidson, Felix Bongomin, Diamantis Kofteridis
Interdisciplinary Perspectives on Infectious Diseases.2022; 2022: 1. CrossRef - Diabetes, obesity, metabolism, and SARS-CoV-2 infection: the end of the beginning
Daniel J. Drucker
Cell Metabolism.2021; 33(3): 479. CrossRef - Effects of a DPP-4 Inhibitor and RAS Blockade on Clinical Outcomes of Patients with Diabetes and COVID-19
Sang Youl Rhee, Jeongwoo Lee, Hyewon Nam, Dae-Sung Kyoung, Dong Wook Shin, Dae Jung Kim
Diabetes & Metabolism Journal.2021; 45(2): 251. CrossRef - COVID-19 vaccine acceptance among high-risk populations in Uganda
Felix Bongomin, Ronald Olum, Irene Andia-Biraro, Frederick Nelson Nakwagala, Khalid Hudow Hassan, Dianah Rhoda Nassozi, Mark Kaddumukasa, Pauline Byakika-Kibwika, Sarah Kiguli, Bruce J. Kirenga
Therapeutic Advances in Infectious Disease.2021; 8: 204993612110243. CrossRef - Caracterización clínica, según niveles de glucemia, de pacientes hospitalizados por COVID-19: serie de casos
Irene Stulin, Maria Montes de Oca, Gabriela Blanco, Laura Sánchez, Isabel-Carlota Silva, Jennireth Quevedo, Maria Cristina Arvelo, Nathalia Valera, Irene Papa, Hospital Centro Médico de Caracas, Caracas, Venezuela Bacci, Fátima de Abreu, Héctor Villarroel
Investigación Clínica.2021; 62: 27. CrossRef - COVID-19 Vaccination for Endocrine Patients: A Position Statement from the Korean Endocrine Society
Cheol Ryong Ku, Kyong Yeun Jung, Chang Ho Ahn, Jun Sung Moon, Ju Hee Lee, Eun Heui Kim, Hyemi Kwon, Hee Kyung Kim, Sunghwan Suh, Sangmo Hong, Jeonghoon Ha, Eun Roh, Jin Hwa Kim, Mi-kyung Kim
Endocrinology and Metabolism.2021; 36(4): 757. CrossRef - Diabetes Mellitus and COVID-19: Review Article
Mahmoud Nassar, Ahmed Daoud, Nso Nso, Luis Medina, Victoria Ghernautan, Harangad Bhangoo, Andrew Nyein, Mahmoud Mohamed, Ahmed Alqassieh, Karim Soliman, Mostafa Alfishawy, Issac Sachmechi, Anoop Misra
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2021; 15(6): 102268. CrossRef - Dissection of non-pharmaceutical interventions implemented by Iran, South Korea, and Turkey in the fight against COVID-19 pandemic
Mohammad Keykhaei, Sogol Koolaji, Esmaeil Mohammadi, Reyhaneh Kalantar, Sahar Saeedi Moghaddam, Arya Aminorroaya, Shaghayegh Zokaei, Sina Azadnajafabad, Negar Rezaei, Erfan Ghasemi, Nazila Rezaei, Rosa Haghshenas, Yosef Farzi, Sina Rashedi, Bagher Larijan
Journal of Diabetes & Metabolic Disorders.2021; 20(2): 1919. CrossRef - A Systematic Review and Meta-analysis of Diabetes Associated Mortality in Patients with COVID-19
Puneeta Gupta, Meeta Gupta, Neena KAtoch, Ketan Garg, Bhawna Garg
International Journal of Endocrinology and Metabolism.2021;[Epub] CrossRef - Diabetes, Obesity, and COVID-19
Sang Youl Rhee
The Journal of Korean Diabetes.2021; 22(3): 174. CrossRef - Diabetes, hypertension, body mass index, smoking and COVID-19-related mortality: a systematic review and meta-analysis of observational studies
Yahya Mahamat-Saleh, Thibault Fiolet, Mathieu Edouard Rebeaud, Matthieu Mulot, Anthony Guihur, Douae El Fatouhi, Nasser Laouali, Nathan Peiffer-Smadja, Dagfinn Aune, Gianluca Severi
BMJ Open.2021; 11(10): e052777. CrossRef - Independent Impact of Diabetes on the Severity of Coronavirus Disease 2019 in 5,307 Patients in South Korea: A Nationwide-Cohort Study (Diabetes Metab J 2020;44:737-46)
Kyuho Kim, Tae Jung Oh
Diabetes & Metabolism Journal.2020; 44(6): 938. CrossRef
- Impact of COVID-19 on the Microbiome and Inflammatory Status of Type 2 Diabetes Patients
- Cardiovascular Risk/Epidemiology
-
- Associations among Obesity Degree, Glycemic Status, and Risk of Heart Failure in 9,720,220 Korean Adults
- Eun-Jung Rhee, Hyemi Kwon, Se Eun Park, Kyung-Do Han, Yong-Gyu Park, Yang-Hyun Kim, Won-Young Lee
- Diabetes Metab J. 2020;44(4):592-601. Published online April 20, 2020
- DOI: https://doi.org/10.4093/dmj.2019.0104
- Correction in: Diabetes Metab J 2020;44(5):783
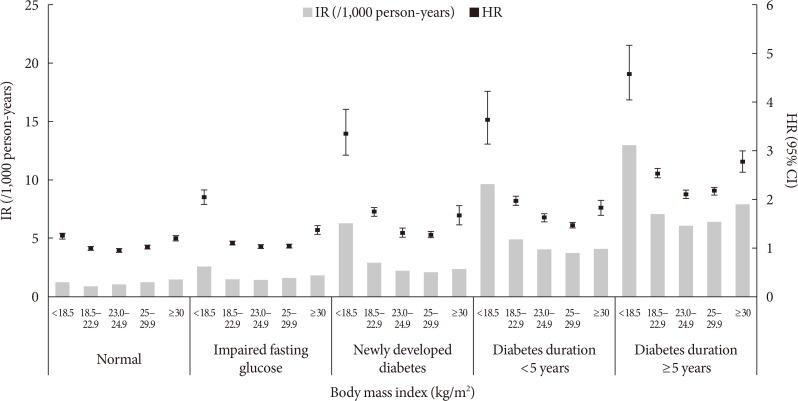
- 6,650 View
- 142 Download
- 16 Web of Science
- 19 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub Background Recent studies suggest an association between diabetes and increased risk of heart failure (HF). However, the associations among obesity status, glycemic status, and risk of HF are not known. In this study, we analyzed whether the risk of HF increases in participants according to baseline glycemic status and whether this increased risk is associated with obesity status.
Methods We analyzed the risk of HF according to baseline glycemic status (normoglycemia, impaired fasting glucose [IFG], and diabetes) in 9,720,220 Koreans who underwent Korean National Health Screening in 2009 without HF at baseline with a median follow-up period of 6.3 years. The participants were divided into five and six groups according to baseline body mass index (BMI) and waist circumference, respectively.
Results Participants with IFG and those with diabetes showed a 1.08- and 1.86-fold increased risk of HF, respectively, compared to normoglycemic participants. Compared to the normal weight group (BMI, 18.5 to 22.9 kg/m2), the underweight group (BMI <18.5 kg/m2) showed a 1.7-fold increased risk of HF, and those with BMI ≥30 kg/m2 showed a 1.1-fold increased risk of HF, suggesting a J-shaped association with BMI. When similar analyses were performed for different glycemic statuses, the J-shaped association between BMI and HF risk was consistently observed in both groups with and without diabetes.
Conclusion Participants with IFG and diabetes showed a significantly increased HF risk compared to normoglycemic participants. This increased risk of HF was mostly prominent in underweight and class II obese participants than in participants with normal weight.
-
Citations
Citations to this article as recorded by- Association between underweight and risk of heart failure in diabetes patients
Tae Kyung Yoo, Kyung‐Do Han, Eun‐Jung Rhee, Won‐Young Lee
Journal of Cachexia, Sarcopenia and Muscle.2024; 15(2): 671. CrossRef - Big Data Research in the Field of Endocrine Diseases Using the Korean National Health Information Database
Sun Wook Cho, Jung Hee Kim, Han Seok Choi, Hwa Young Ahn, Mee Kyoung Kim, Eun Jung Rhee
Endocrinology and Metabolism.2023; 38(1): 10. CrossRef - Research on obesity using the National Health Information Database: recent trends
Eun-Jung Rhee
Cardiovascular Prevention and Pharmacotherapy.2023; 5(2): 35. CrossRef - Impact of mental disorders on the risk of heart failure among Korean patients with diabetes: a cohort study
Tae Kyung Yoo, Kyung-Do Han, Eun-Jung Rhee, Won-Young Lee
Cardiovascular Diabetology.2023;[Epub] CrossRef - Differential Impact of Obesity on the Risk of Diabetes Development in Two Age Groups: Analysis from the National Health Screening Program
Tae Kyung Yoo, Kyung-Do Han, Yang-Hyun Kim, Ga Eun Nam, Sang Hyun Park, Eun-Jung Rhee, Won-Young Lee
Diabetes & Metabolism Journal.2023; 47(6): 846. CrossRef - Characterization of the oxidative stress and inflammatory markers in metabolically healthy obese individuals
Hazhmat Ali
Al-Kufa University Journal for Biology.2023; 15(3): 28. CrossRef - The Influence of Obesity and Metabolic Health on Vascular Health
Eun-Jung Rhee
Endocrinology and Metabolism.2022; 37(1): 1. CrossRef - Changes in Patterns of Physical Activity and Risk of Heart Failure in Newly Diagnosed Diabetes Mellitus Patients
Inha Jung, Hyemi Kwon, Se Eun Park, Kyung-Do Han, Yong-Gyu Park, Eun-Jung Rhee, Won-Young Lee
Diabetes & Metabolism Journal.2022; 46(2): 327. CrossRef - Evaluating Triglyceride and Glucose Index as a Simple and Easy-to-Calculate Marker for All-Cause and Cardiovascular Mortality
Kyung-Soo Kim, Sangmo Hong, You-Cheol Hwang, Hong-Yup Ahn, Cheol-Young Park
Journal of General Internal Medicine.2022; 37(16): 4153. CrossRef - Impact of hypoglycemia at the time of hospitalization for heart failure from emergency department on major adverse cardiovascular events in patients with and without type 2 diabetes
Seon-Ah Cha, Jae-Seung Yun, Gee-Hee Kim, Yu-Bae Ahn
Cardiovascular Diabetology.2022;[Epub] CrossRef - Insulin resistance and heart failure with preserved ejection fraction. Pathogenetic and therapeutic crossroads
O. V. Tsygankova, N. E. Evdokimova, V. V. Veretyuk, L. D. Latyntseva, A. S. Ametov
Diabetes mellitus.2022; 25(6): 535. CrossRef - The association between metabolic syndrome and heart failure in middle-aged male and female: Korean population-based study of 2 million individuals
Tae-Eun Kim, Hyeongsu Kim, JiDong Sung, Duk-Kyung Kim, Myoung-Soon Lee, Seong Woo Han, Hyun-Joong Kim, Sung Hea Kim, Kyu-Hyung Ryu
Epidemiology and Health.2022; 44: e2022078. CrossRef - Diabetes and Heart Failure
Eun-Jung Rhee
The Journal of Korean Diabetes.2021; 22(1): 12. CrossRef - Prediabetes and the risk of heart failure: A meta‐analysis
Xiaoyan Cai, Xiong Liu, Lichang Sun, Yiting He, Sulin Zheng, Yang Zhang, Yuli Huang
Diabetes, Obesity and Metabolism.2021; 23(8): 1746. CrossRef - Diabetes and Heart Failure
Eun-Jung Rhee
Cardiovascular Prevention and Pharmacotherapy.2021; 3(2): 21. CrossRef - Effects of Lipid Overload on Heart in Metabolic
Diseases
An Yan, Guinan Xie, Xinya Ding, Yi Wang, Liping Guo
Hormone and Metabolic Research.2021; 53(12): 771. CrossRef - Obesity Degree and Glycemic Status: Factors That Should Be Considered in Heart Failure
Hye Soon Kim
Diabetes & Metabolism Journal.2020; 44(4): 529. CrossRef - Letter: Associations among Obesity Degree, Glycemic Status, and Risk of Heart Failure in 9,720,220 Korean Adults (Diabetes Metab J 2020;44:592-601)
Darae Kim
Diabetes & Metabolism Journal.2020; 44(5): 777. CrossRef - Response: Associations among Obesity Degree, Glycemic Status, and Risk of Heart Failure in 9,720,220 Korean Adults (Diabetes Metab J 2020;44:592-601)
Eun-Jung Rhee, Won-Young Lee
Diabetes & Metabolism Journal.2020; 44(5): 781. CrossRef
- Association between underweight and risk of heart failure in diabetes patients
- Epidemiology
- Relation between Baseline Height and New Diabetes Development: A Nationwide Population-Based Study
- Eun-Jung Rhee, Jung-Hwan Cho, Hyemi Kwon, Se-Eun Park, Jin-Hyung Jung, Kyung-Do Han, Yong-Gyu Park, Yang-Hyun Kim, Won-Young Lee
- Diabetes Metab J. 2019;43(6):794-803. Published online March 22, 2019
- DOI: https://doi.org/10.4093/dmj.2018.0184
- 4,879 View
- 59 Download
- 8 Web of Science
- 10 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Short stature and leg length are associated with risk of diabetes and obesity. However, it remains unclear whether this association is observed in Asians. We evaluated the association between short stature and increased risk for diabetes using the Korean National Health Screening (KNHS) dataset.
Methods We assessed diabetes development in 2015 in 21,122,422 non-diabetic Koreans (mean age 43 years) enrolled in KNHS from 2009 to 2012 using International Classification of Diseases 10th (ICD-10) code and anti-diabetic medication prescription. Risk was measured in age- and sex-dependent quintile groups of baseline height (20 to 39, 40 to 59, ≥60 years).
Results During median 5.6-year follow-up, 532,918 cases (2.5%) of diabetes occurred. The hazard ratio (HR) for diabetes development gradually increased from the 5th (reference) to 1st quintile group of baseline height after adjustment for confounding factors (1.000, 1.076 [1.067 to 1.085], 1.097 [1.088 to 1.107], 1.141 [1.132 to 1.151], 1.234 [1.224 to 1.244]), with similar results in analysis by sex. The HR per 5 cm height increase was lower than 1.00 only in those with fasting blood glucose (FBG) below 100 mg/dL (0.979 [0.975 to 0.983]), and in lean individuals (body mass index [BMI] 18.5 to 23 kg/m2: 0.993 [0.988 to 0.998]; BMI <18.5 kg/m2: 0.918 [0.9 to 0.935]).
Conclusion Height was inversely associated with diabetes risk in this nationwide study of Korean adults. This association did not differ by sex, and was significant in lean individuals and those with normal FBG levels.
-
Citations
Citations to this article as recorded by- Association between underweight and risk of heart failure in diabetes patients
Tae Kyung Yoo, Kyung‐Do Han, Eun‐Jung Rhee, Won‐Young Lee
Journal of Cachexia, Sarcopenia and Muscle.2024; 15(2): 671. CrossRef - Upper arm length and knee height are associated with diabetes in the middle-aged and elderly: evidence from the China Health and Retirement Longitudinal Study
Bingjie He, Zhengyang Li, Lu Xu, Lili Liu, Shengfeng Wang, Siyan Zhan, Yongfeng Song
Public Health Nutrition.2023; 26(1): 190. CrossRef - Anthropometric indexes and cardiovascular risk in Ecuadorian university students: A comparison with international references
Silvia Cáceres-Vinueza, Evelyn Frias-Toral, Rosario Suárez, Jorge Daher-Nader, Enrique Flor-Muñoz, Mirna Márquez-Vinueza, Luisa Valeria Guevara-Flores, Yan Duarte-Vera
Bionatura.2023; 8(3): 1. CrossRef - Assessment of common risk factors of diabetes and chronic kidney disease: a Mendelian randomization study
Shuwu Zhao, Yiming Li, Chen Su
Frontiers in Endocrinology.2023;[Epub] CrossRef - Inverse association between adult height and diabetes risk in a cohort study of Chinese population
Xiaoli Li, Tiantian Cheng, Lina Leng, Guangyao Song, Huijuan Ma
Scientific Reports.2023;[Epub] CrossRef - Gender Differences Between the Phenotype of Short Stature and the Risk of Diabetes Mellitus in Chinese Adults: A Population-Based Cohort Study
Wei Song, Yaqin Hu, Jiao Yuan, Ying Wei, Zongyou Cheng, Jingdong Liu, Jixiong Xu, Xiaoyu Wang
Frontiers in Endocrinology.2022;[Epub] CrossRef - No association between body height and metabolic risk factors in historically short height Asian Indian tribes
Binu Dorjee, Jaydip Sen, Mithun Das, Kaushik Bose, Christiane Scheffler, Gautam Kumar Kshatriya
Human Biology and Public Health.2022;[Epub] CrossRef - Newly diagnosed diabetes has high risk for cardiovascular outcome in ischemic stroke patients
Kyung-Hee Cho, Sun U. Kwon, Ji Sung Lee, Sungwook Yu, A-Hyun Cho
Scientific Reports.2021;[Epub] CrossRef - Risk of Diabetes in Subjects with Positive Fecal Immunochemical Test: A Nationwide Population-Based Study
Kwang Woo Kim, Hyun Jung Lee, Kyungdo Han, Jung Min Moon, Seung Wook Hong, Eun Ae Kang, Jooyoung Lee, Hosim Soh, Seong-Joon Koh, Jong Pil Im, Joo Sung Kim
Endocrinology and Metabolism.2021; 36(5): 1069. CrossRef - The use of Broca index to assess cut- off points for overweight in adults: A short review
Irakoze Laurent, Manirakiza Astère, Banderembako Paul, Nkengurutse Liliane, Yue Li, Qingfeng Cheng, Qifu Li, Xiaoqiu Xiao
Reviews in Endocrine and Metabolic Disorders.2020; 21(4): 521. CrossRef
- Association between underweight and risk of heart failure in diabetes patients
- Obesity and Metabolic Syndrome
-
- The Risk of Myocardial Infarction and Ischemic Stroke According to Waist Circumference in 21,749,261 Korean Adults: A Nationwide Population-Based Study
- Jung-Hwan Cho, Eun-Jung Rhee, Se-Eun Park, Hyemi Kwon, Jin-Hyung Jung, Kyung-Do Han, Yong-Gyu Park, Hye Soon Park, Yang-Hyun Kim, Soon-Jib Yoo, Won-Young Lee
- Diabetes Metab J. 2019;43(2):206-221. Published online December 27, 2018
- DOI: https://doi.org/10.4093/dmj.2018.0039
- 5,620 View
- 102 Download
- 22 Web of Science
- 23 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader Background Waist circumference (WC) is a well-known obesity index that predicts cardiovascular disease (CVD). We studied the relationship between baseline WC and development of incident myocardial infarction (MI) and ischemic stroke (IS) using a nationwide population-based cohort, and evaluated if its predictability is better than body mass index (BMI).
Methods Our study included 21,749,261 Koreans over 20 years of age who underwent the Korean National Health Screening between 2009 and 2012. The occurrence of MI or IS was investigated until the end of 2015 using National Health Insurance Service data.
Results A total of 127,289 and 181,637 subjects were newly diagnosed with MI and IS. The incidence rate and hazard ratio of MI and IS increased linearly as the WC level increased, regardless of adjustment for BMI. When the analyses were performed according to 11 groups of WC, the lowest risk of MI was found in subjects with WC of 70 to 74.9 and 65 to 69.9 cm in male and female, and the lowest risk of IS in subjects with WC of 65 to 69.9 and 60 to 64.9 cm in male and female, respectively. WC showed a better ability to predict CVD than BMI with smaller Akaike information criterion. The optimal WC cutoffs were 84/78 cm for male/female for predicting MI, and 85/78 cm for male/female for predicting IS.
Conclusion WC had a significant linear relationship with the risk of MI and IS and the risk began to increase from a WC that was lower than expected.
-
Citations
Citations to this article as recorded by- Usefulness of New Criteria for Metabolic Syndrome Optimized for Prediction of Cardiovascular Diseases in Japanese
Yurie Yamazaki, Kazuya Fujihara, Takaaki Sato, Mayuko Harada Yamada, Yuta Yaguchi, Yasuhiro Matsubayashi, Takaho Yamada, Satoru Kodama, Kiminori Kato, Hitoshi Shimano, Hirohito Sone
Journal of Atherosclerosis and Thrombosis.2024; 31(4): 382. CrossRef - Association between body composition and subsequent cardiovascular diseases among 5-year breast cancer survivors
Ji Soo Kim, Jihun Song, Seulggie Choi, Sung Min Kim, Young Jun Park, Sun Jae Park, Yoosun Cho, Yun Hwan Oh, Seogsong Jeong, Kyae Hyung Kim, Sang Min Park
Nutrition, Metabolism and Cardiovascular Diseases.2024;[Epub] CrossRef - Body mass index, waist circumference and cardiovascular diseases in transitional ages (40 and 66 years)
Jung Eun Yoo, Kyungdo Han, Jin‐Hyung Jung, Yang‐Im Hur, Yang Hyun Kim, Eun Sook Kim, Jang Won Son, Eun‐Jung Rhee, Won‐Young Lee, Ga Eun Nam
Journal of Cachexia, Sarcopenia and Muscle.2023; 14(1): 369. CrossRef - Risk factors for stroke among anthropometric indices and lipid profiles in the Korean population: a large-scale cross-sectional study
Mi Hong Yim, Young Ju Jeon, Bum Ju Lee
Scientific Reports.2023;[Epub] CrossRef - Big Data Research in the Field of Endocrine Diseases Using the Korean National Health Information Database
Sun Wook Cho, Jung Hee Kim, Han Seok Choi, Hwa Young Ahn, Mee Kyoung Kim, Eun Jung Rhee
Endocrinology and Metabolism.2023; 38(1): 10. CrossRef - Research on obesity using the National Health Information Database: recent trends
Eun-Jung Rhee
Cardiovascular Prevention and Pharmacotherapy.2023; 5(2): 35. CrossRef - Association between the weight-adjusted waist index and stroke: a cross-sectional study
Jiayi Ye, Yanjie Hu, Xinrong Chen, Zhe Yin, Xingzhu Yuan, Liping Huang, Ka Li
BMC Public Health.2023;[Epub] CrossRef - Increased risk of ischemic stroke associated with elevated gamma-glutamyl transferase level in adult cancer survivors: a population-based cohort study
Kyuwoong Kim, Hyeyun Jung, Edvige Di Giovanna, Tae Joon Jun, Young-Hak Kim
Scientific Reports.2023;[Epub] CrossRef - Changes in body composition and subsequent cardiovascular disease risk among 5-year breast cancer survivors
Ji Soo Kim, Jihun Song, Seulggie Choi, Sang Min Park
Frontiers in Cardiovascular Medicine.2023;[Epub] CrossRef - Association between Stroke and Abdominal Obesity in the Middle-Aged and Elderly Korean Population: KNHANES Data from 2011–2019
Jong Yeon Kim, Sung Min Cho, Youngmin Yoo, Taesic Lee, Jong Koo Kim
International Journal of Environmental Research and Public Health.2022; 19(10): 6140. CrossRef - Prevalence of metabolic syndrome and related factors in a large sample of antipsychotic naïve patients with first-episode psychosis: Baseline results from the PAFIP cohort
Nathalia Garrido-Torres, Miguel Ruiz-Veguilla, Luis Alameda, Manuel Canal-Rivero, María Juncal Ruiz, Marcos Gómez-Revuelta, Rosa Ayesa-Arriola, Ana Rubio-García, Benedicto Crespo-Facorro, Javier Vázquez-Bourgon
Schizophrenia Research.2022; 246: 277. CrossRef - Development and validation of risk prediction models for stroke and mortality among patients with type 2 diabetes in northern China
X. Shao, H. Liu, F. Hou, Y. Bai, Z. Cui, Y. Lin, X. Jiang, P. Bai, Y. Wang, Y. Zhang, C. Lu, H. Liu, S. Zhou, P. Yu
Journal of Endocrinological Investigation.2022; 46(2): 271. CrossRef - Neck circumference for predicting the occurrence of future cardiovascular events: A 7.6-year longitudinal study
Tingting Hu, Yun Shen, Weijie Cao, Yiting Xu, Yufei Wang, Xiaojing Ma, Yuqian Bao
Nutrition, Metabolism and Cardiovascular Diseases.2022; 32(12): 2830. CrossRef - A prospective study of waist circumference trajectories and incident cardiovascular disease in China: the Kailuan Cohort Study
Liang Wang, Yujin Lee, Yuntao Wu, Xinyuan Zhang, Cheng Jin, Zhe Huang, Yixin Wang, Zhiyi Wang, Penny Kris-Etherton, Shouling Wu, Xiang Gao
The American Journal of Clinical Nutrition.2021; 113(2): 338. CrossRef - The Repeatedly Elevated Fatty Liver Index Is Associated With Increased Mortality: A Population-Based Cohort Study
Chang-Hoon Lee, Kyung-Do Han, Da Hye Kim, Min-Sun Kwak
Frontiers in Endocrinology.2021;[Epub] CrossRef - Obesity Degree and Glycemic Status: Factors That Should Be Considered in Heart Failure
Hye Soon Kim
Diabetes & Metabolism Journal.2020; 44(4): 529. CrossRef - Exposure-weighted scoring for metabolic syndrome and the risk of myocardial infarction and stroke: a nationwide population-based study
Eun Young Lee, Kyungdo Han, Da Hye Kim, Yong-Moon Park, Hyuk-Sang Kwon, Kun-Ho Yoon, Mee Kyoung Kim, Seung-Hwan Lee
Cardiovascular Diabetology.2020;[Epub] CrossRef - Predicting the Development of Myocardial Infarction in Middle-Aged Adults with Type 2 Diabetes: A Risk Model Generated from a Nationwide Population-Based Cohort Study in Korea
Seung-Hwan Lee, Kyungdo Han, Hun-Sung Kim, Jae-Hyoung Cho, Kun-Ho Yoon, Mee Kyoung Kim
Endocrinology and Metabolism.2020; 35(3): 636. CrossRef - Obesity Fact Sheet in Korea, 2018: Data Focusing on Waist Circumference and Obesity-Related Comorbidities
Ga Eun Nam, Yang-Hyun Kim, Kyungdo Han, Jin-Hyung Jung, Yong Gyu Park, Kwan-Woo Lee, Eun-Jung Rhee, Jang Won Son, Seong-Su Lee, Hyuk-Sang Kwon, Won-Young Lee, Soon Jib Yoo
Journal of Obesity & Metabolic Syndrome.2019; 28(4): 236. CrossRef - Simply the Best: Anthropometric Indices for Predicting Cardiovascular Disease
Jie-Eun Lee
Diabetes & Metabolism Journal.2019; 43(2): 156. CrossRef - Association and Interaction Analysis of Lipid Accumulation Product with Impaired Fasting Glucose Risk: A Cross-Sectional Survey
Jian Song, Xue Chen, Yuhong Jiang, Jing Mi, Yuyuan Zhang, Yingying Zhao, Xuesen Wu, Huaiquan Gao
Journal of Diabetes Research.2019; 2019: 1. CrossRef - Letter: Association of Z-Score of the Log-Transformed A Body Shape Index with Cardiovascular Disease in People Who Are Obese but Metabolically Healthy: The Korea National Health and Nutrition Examination Survey 2007-2010 (J Obes Metab Syndr 2018;27:158-65
Eun-Jung Rhee
Journal of Obesity & Metabolic Syndrome.2019; 28(2): 139. CrossRef - Response: The Differential Association between Muscle Strength and Diabetes Mellitus According to the Presence or Absence of Obesity (J Obes Metab Syndr 2019;28:46-52)
Bo Kyung Koo
Journal of Obesity & Metabolic Syndrome.2019; 28(4): 297. CrossRef
- Usefulness of New Criteria for Metabolic Syndrome Optimized for Prediction of Cardiovascular Diseases in Japanese

 KDA
KDA
 First
First Prev
Prev





